
In the rehab and strength and conditioning communities, it is widely accepted that programming within a stress-recovery-adaptation (SRA) cycle is an effective methodology for creating sport-specific, targeted adaptations in our high-performance and tactical athletes. Considering the connections between movement quality and stress/physiology that have been established in research, it may be beneficial to use assessment of movement quality (motion analysis) to determine where an athlete’s movement patterns are revealing current stress on the system.
Based on this objective data for each athlete, we can then set specific training and rehab goals and develop highly individualized programming to facilitate precise positive adaptations. Motion analysis also gives us a measurable way to track athlete progress over time—a valuable tool to validate the effectiveness of programming efforts.
Programming Within an SRA Cycle
While many coaches and therapists agree with SRA ideology for promoting positive performance adaptations, few truly understand the underlying neurological mechanisms involved and how to begin designing programs to maximize positive adaptations based on these principles.
Traditionally, the focus of the SRA cycle has been on the physical aspects of stress, recovery, and adaptation. This makes sense in our industry, as improving motor performance and physical readiness is the goal of all training programs, and it is typically the most observable of the adaptations that occur within the cycle (e.g., increased strength, speed, endurance). However, the ability of our bodies to detect, withstand, and adapt from stress is largely a neurological process, primarily dictated by healthy structure and function of the vagus nerve. In order to optimize our athletes’ ability to adapt from stress, we need a deeper understanding of the systemic impacts of stress on the body—and particularly the impacts that stress has on motor performance. Let’s start by looking more closely at the SRA cycle.
To optimize our athletes’ ability to adapt from stress, we need a deeper understanding of the systemic impacts of stress on the body—particularly the impacts it has on motor performance. Share on X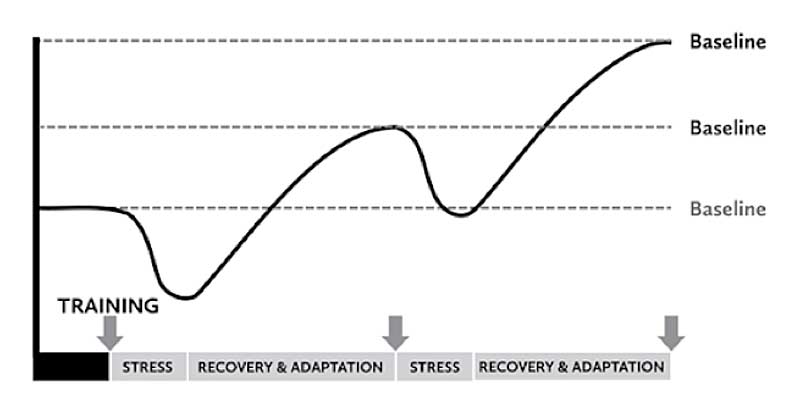
The process of deviating from baseline and returning is commonly described as resilience. The overall goal of the SRA cycle is to prescribe the optimal amount of stress and recovery to the individual athlete, so that the result is a measurable positive adaptation in the targeted baseline skill set. We can strategically apply stress and recovery principles within programming to continuously facilitate positive performance adaptations while simultaneously improving baseline tolerance for the applied stress.
Another important note from the graph is that once the stress is applied, we see a temporary decrease in the targeted skill set. When appropriately assessing our athletes using motion analysis, we can detect stress as a decline in movement quality from the athlete’s baseline. This decline in movement quality (a readiness indicator) is a normal part of our systemic stress response and a valuable clue as to when our programming focus should shift to support recovery and facilitate positive adaptation.
The Vagus Nerve, Stress, and Movement
The vagus nerve (cranial nerve 10) is the longest and most complex of the 12 cranial nerves. It emerges directly from the brain and has both sensory and motor functions. One of the primary roles of the vagus nerve is to modulate activity within the autonomic nervous system, specifically regulating sympathetic (fight-or-flight)/parasympathetic (recovery/relaxation) tone.
The vagus nerve also controls heart rate variability (HRV), which is a measure of a person’s ability to adapt to stress. The sensory and motor fibers of the vagus nerve travel throughout the fascia system, and therefore structure and function of the vagus nerve are largely dependent on a healthy musculoskeletal system and efficient movement patterns. In this sense, when used appropriately, movement has the potential to regulate our physiology and promote positive adaptations from stress. Conversely, movement, especially loaded movement, also has the potential to inhibit positive adaptations when applied without mindfulness regarding the current level of stress. Let’s go a little deeper.
Conversely, movement, especially loaded movement, also has the potential to inhibit positive adaptations when applied without mindfulness regarding the current level of stress. Share on XThe vagus nerve acts as the body’s surveillance system, designed to detect any imbalance or threat to homeostasis, both internally and externally. A threat to homeostasis can be anything from an increase in heart rate during exercise to a heavy external load or an actual physical injury. Any time a threat is detected, the vagus nerve sends warning signals to the brain, which triggers a series of cellular, chemical, and physical reactions to restore homeostasis within the body. This series of reactions to return an individual to baseline is called allostasis.
When an athlete is placed under stress and they are in an allostatic response, we should expect to see a temporary decline in motor functions (recall the graph). Once the person reaches their homeostatic baseline through recovery, the vagus nerve sends signals to the brain that the threat has passed, and the nervous system is in a prime position to integrate the stressful experience and create positive physical adaptations specific to the type of stress. In the case of a stressful situation turning into a positive adaptation, the stress is classified as eustress (good stress/adaptive stress). This is the goal of training within an SRA cycle.
If the athlete does not adequately recover and never reaches their baseline, however, the stress response continues—then, they are unable to transform the experience into a positive adaptation. A positive adaptation cannot occur until the vagus nerve sends signals of safety to the brain. If the stress response continues long term, with no return to baseline, the athlete is at greater risk for negative outcomes, such as injury and even illness. Our bodies are made to withstand short periods of stress, not chronic stress. In the case of an athlete having inadequate recovery, the stress would become distress (negative/maladaptive stress) and would be visible over time with faulty movement patterns and compensations.
One of the most important points from above is that if an athlete is in stress, their motor performance and movement quality will inevitably suffer (decrease from baseline on SRA graph). This provides implications for professionals working with tactical athletes and high-performance athletes to be assessing movement quality at various intervals, to monitor the athlete’s adaptive response to prescriptive programming and applied stress.
Note: Understanding the difference between eustress and distress as it relates to performance is especially important for professionals working with tactical populations, where operational stress puts these athletes at higher risk for allostatic overload (chronic inability to return to baseline). Research is showing that these athletes demonstrate a decline in motor performance and readiness indicators long after intense operational training has ended, and even longer after combat deployments. For best practice, this should be considered when prescribing stress and recovery programming for this population.
Motion Analysis for High-Performance and Tactical Athletes
We’ve established that using standardized assessments of motor performance and physical readiness enables therapists and coaches to develop highly individualized prescriptive programming within a stress-recovery-adaptation cycle. But how do we actually perform a movement assessment? While most coaches rely on their own trained eye to spot imbalances in the musculoskeletal system and faulty movement patterns, recent advances in the fields of bioengineering and sports science have led to the development of high-tech motion analysis equipment, which is slowly being integrated into the industry by various professionals.
Technology from BTS Bioengineering allows for the assessment of neuromuscular activation, multiplanar accelerations/rotations, range of motion, and spatiotemporal parameters within a variety of movement patterns. The data provided allows for the most objective assessment of current performance abilities, including where they might fall on the SRA cycle graph. We can then use this information to develop individualized programming to facilitate specific positive performance adaptations.
BTS Bioengineering
BTS Bioengineering is an Italian-based company that has been researching and developing innovative technologies for motion analysis since 1986. BTS has a plethora of options when it comes to motion analysis equipment. At Elite Performance Concepts (EPC), we have 3D motion capture cameras, force plates, wireless EMG sensors, and inertia sensor all from BTS. BTS equipment has been validated and used in peer-reviewed scientific journals—they are truly a leader in the field.
The equipment comes with some protocols that have normative data already within the software (for example, gait and running analysis, vertical jump indexes, drop jump test, and cervical spine test). These tests have been well researched and allow us to see where an athlete’s scores place them when compared with a group of the normal population.
I can pick and choose which assessments will give the best data based on the athlete’s goals and how they are currently presenting, to create a completely individualized assessment. Share on XI have also worked with BTS to create custom EMG and 3D motion capture protocols for squat, deadlift, and bench press. While these protocols do not have normative data, they allow me to assess symmetry throughout a movement pattern, as well as track symmetry over time in response to programming. With all the available testing options, I can pick and choose which assessments will give the best data based on the athlete’s goals and how they are currently presenting, to create a completely individualized assessment.
Case Studies
At EPC, we see two sets of clients:
- Traditional rehab clients. These are people coming to us with a specific injury or issue. On an SRA cycle graph, they would be below their baseline and in stress.
- Athletes. These clients are at their performance baseline and are looking to improve skills related to a specific sport or activity. These individuals would be at their baseline on the SRA curve or maybe a little below baseline if they have been neglecting recovery.
Despite one set of clients coming in with injuries and the other looking to improve baseline performance abilities, both are in a prime position to strategically apply motion analysis and SRA principles to promote positive performance adaptations. Let’s look at the data of two different clients to get a better understanding of how we can use this equipment to program for our athletes within an SRA cycle.
Case Study 1: Rehab Client
The first client that we will look at is a rehab client. This client is an older adult who has remained extremely physically fit throughout her life. Up until earlier this year—when she tore the meniscus in her right knee—she was strength training regularly in the gym. She had the tear repaired surgically and used traditional physical therapy for her rehab. In one session, she had extreme pain when the therapist forced her knee into terminal extension. She has had swelling and pain in the knee ever since, and recently had an MRI that showed two new tears in the same knee. The client is scheduled for another surgical repair in a few weeks.
For her assessment, I chose to do a gait analysis using EMG and inertia sensors. We did two assessments: one with a crutch on the right side and one without the crutch. We wanted to compare her gait with and without the crutch to determine whether she should continue to use it. Our goal was also to get a pre-op analysis to compare postoperatively. Having data to show progress over time can be an extremely valuable tool for the rehab client’s mentality throughout the process.
The BTS protocol that I used for this client is the Freewalk Protocol. This protocol collects data regarding neuromuscular activation through use of 8 EMG (electromyography) sensors and spatiotemporal parameters of the gait cycle via the G-Sensor (inertia sensor). The G-Sensor is placed at the level of the pelvis and measures angular accelerations in three planes of movement, as well as events within the gait cycle. The EMG probes are placed on the following muscles (right and left sides): tibialis anterior, gastrocnemius medialis, rectus femoris, semitendinosus. Gait kinematics have been researched extensively for several decades, and therefore, the protocol has a high level of validity and compares our client’s data to normative data of the general population.
Data Analysis
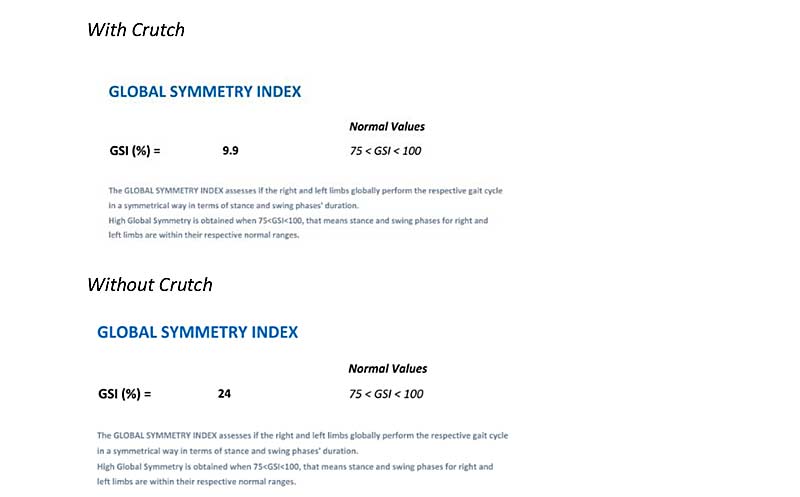
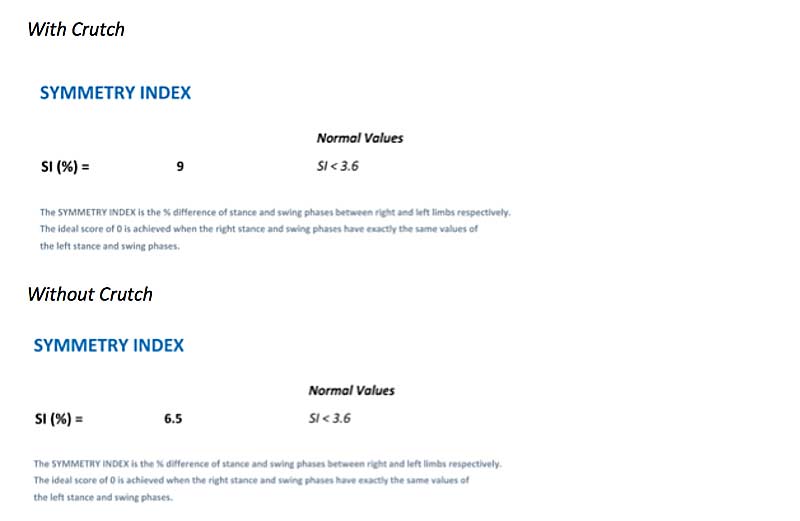
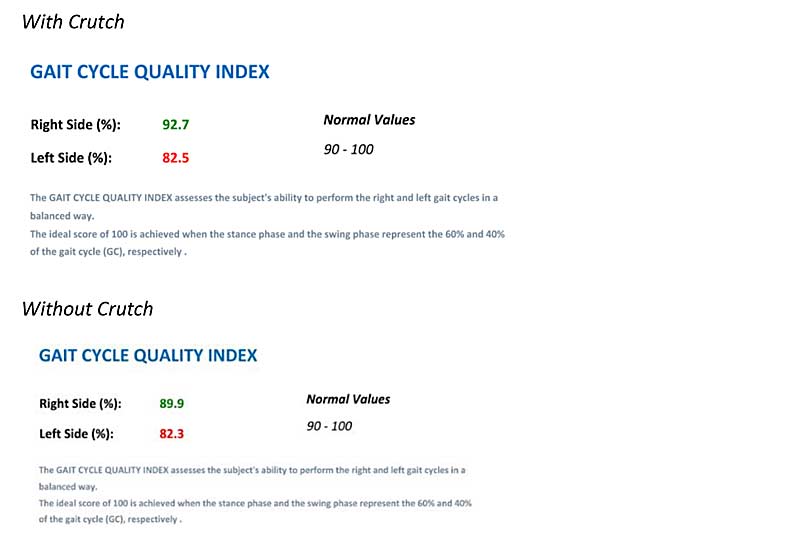
Going through the protocol report, the first aspect of gait that we will look at are temporal parameters collected by the G-Sensor. Events would be things like heel strike, toe-off, single support phase, double support phase, stance, and swing phase. Through data analysis, we get multiple symmetry indexes, which give information about timing of events within the gait cycle compared to normative data. Below, find the symmetry indexes for this client with and without the use of the crutch. There are three indexes provided:
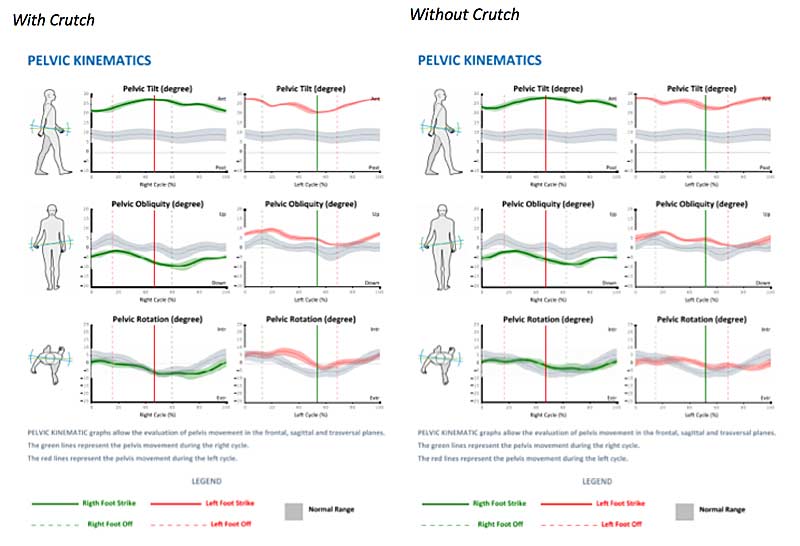
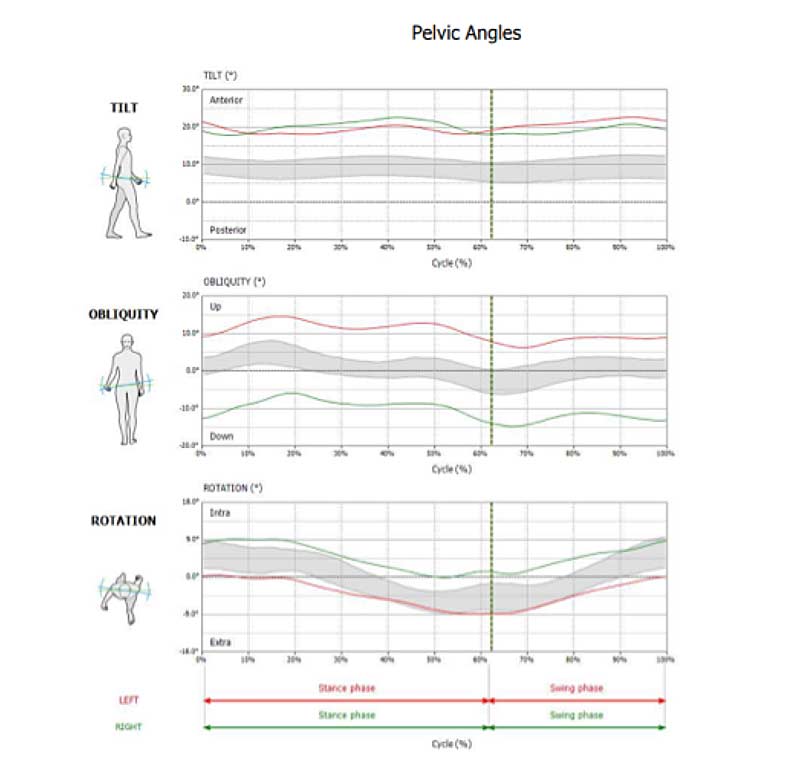
The next part of the report we will look at are the pelvic kinematics. These graphs allow us to evaluate pelvic movements in the frontal, sagittal, and transverse planes. The green graph lines represent data from the right gait cycle, while the red graph lines represent data from the left gait cycle. Normative data is represented by the gray band. Pelvic kinematics that are considered “normal” would fall within the gray band.
Pelvic kinematics for this client were pretty similar with (right side) and without (left side) the crutch. The most significant deviation that we see in this client is excessive anterior tilt throughout the entire gait cycle. The norm for adults is about 10 degrees of anterior tilt throughout the cycle. This client has almost 25 degrees of anterior tilt throughout the gait cycle. She also falls outside of normal range for right and left pelvic obliquity; however, the deviation is not as significant as the anterior tilt.
The last piece of data is the EMG data within the gait cycle. First, we will look at the data from the lower leg. The graphs on top look at timing of the right (green) and left gait cycles (red). The gray part of the graph is when we should see peak EMG activity, such as is seen in the left gastroc both with and without a crutch. We should see almost no activity in the white areas (a flat line). As you can see, there is very little activity in the right lower leg both with and without a crutch. We also see the right gastroc firing in the white areas of the graph, where it should be almost flat.
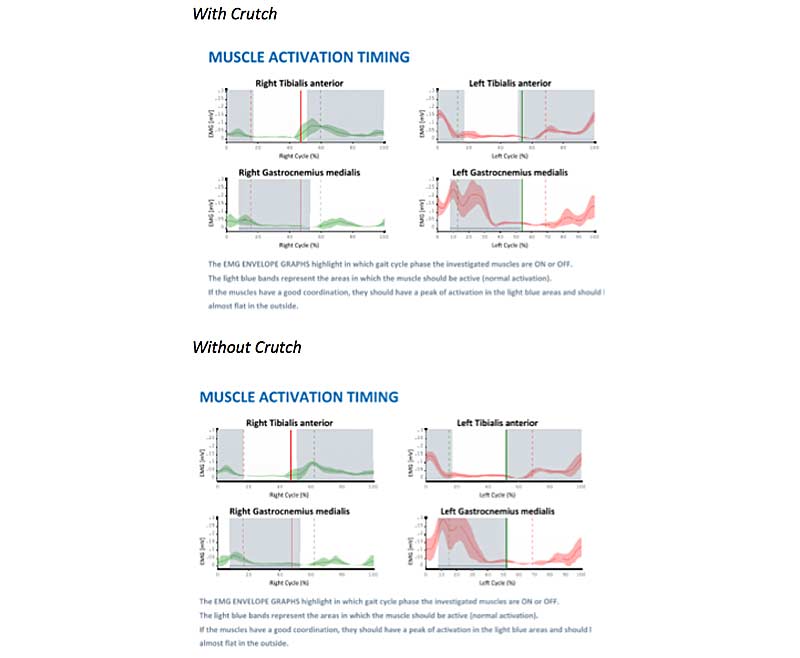
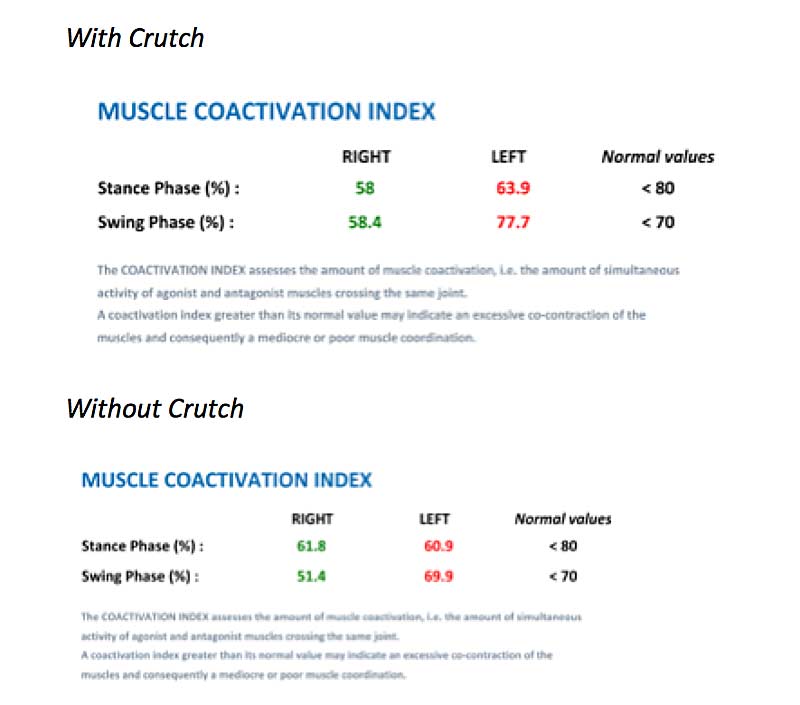
This brings us to the next part of the data, the coactivation index (figure 4).
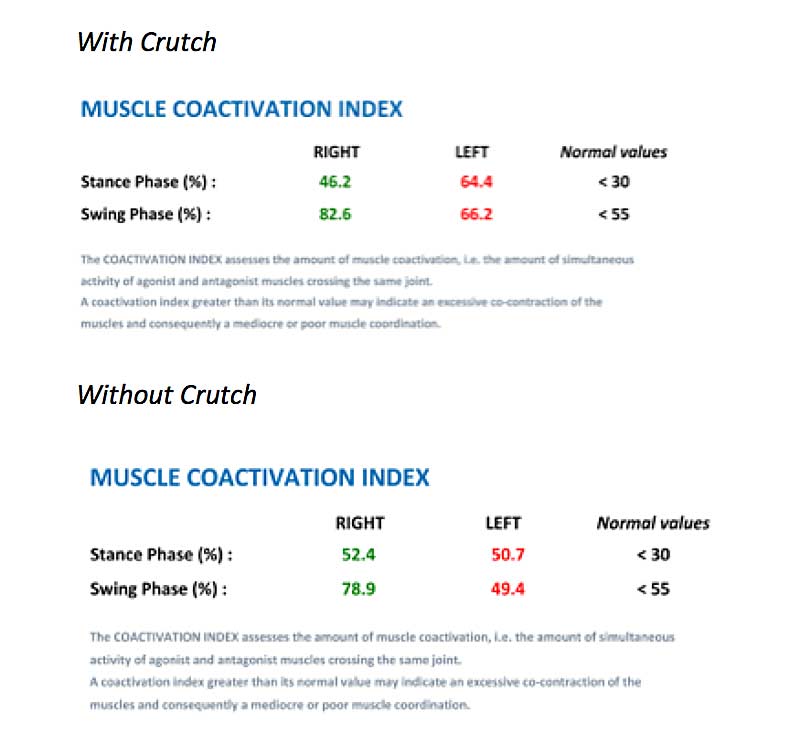
The coactivation index assesses simultaneous agonist and antagonist muscle activation. Normal values are listed in black on the right side. A coactivation index greater than the normal values would indicate co-contraction of agonist and antagonist muscles (gastroc and tibialis), and poor synchronicity of muscle activation within the gait pattern. Both RLE and LLE showed a high level of coactivation in the lower leg throughout the gait cycle both with and without the crutch. This is typical in clients who have an active injury, as it is the body’s way of protecting the joint.
Looking at the EMG data for the upper leg, we see very little activity in the right quadriceps (rectus femoris) both with and without a crutch. We also see excessive hamstring activity bilaterally in white areas, where there should be almost no activity. This is likely a compensation for the lack of rectus fem engagement.
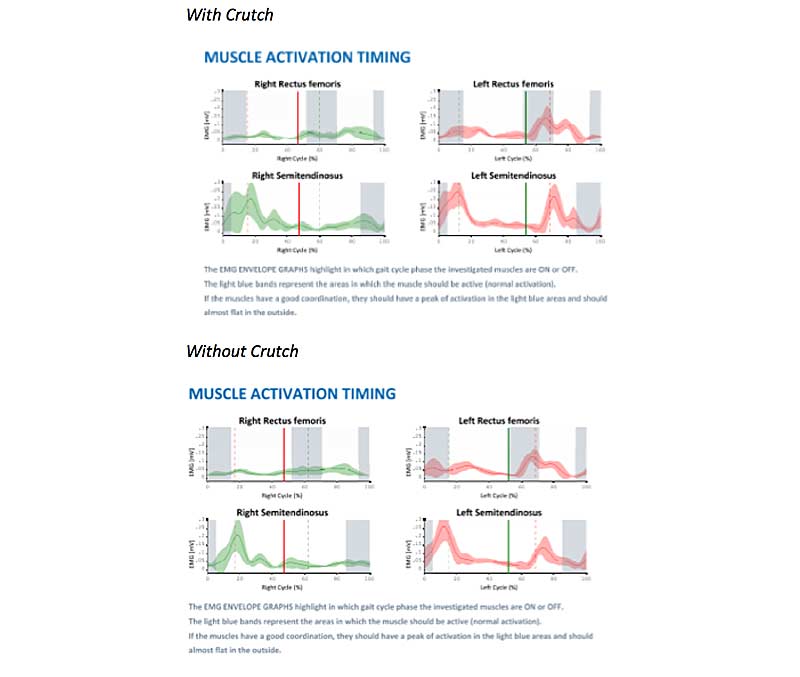
Coactivation indexes both with and without the crutch fell within normal limits (except left swing phase with crutch), indicating no excessive agonist/antagonist co-contraction in the upper leg, bilaterally.
Interpretation of Results
Based on the data, this client did not have a significant difference in gait cycle quality with or without the crutch. However, since she did have slightly better symmetry without the crutch, I recommended she only use the crutch when leaving her house for community ambulation, as it gave her some peace of mind when walking longer distances.
Overall, this client’s assessment reveals a high level of stress within the musculoskeletal system. We see this with poor temporal symmetry, decreased neuromuscular activation in the lower leg and quads, high coactivation within agonist/antagonist muscle groups, and excessive anterior tilt within the pelvis. Based on this data and her presentation as highly anxious regarding this injury and her current quality of life, I would start this client on a rehab program that initially focuses almost entirely on systemic recovery. This client is stressed physically, mentally, and emotionally over this injury, and is well below her functional baseline on the SRA curve.
The recovery methods we use at EPC include:
- Myofascial release therapy/bodywork.
- Movement re-patterning (Masgutova Neurosensorimotor Reflex Integration techniques).
- Sensory integration techniques (MNRI, Safe and Sound Protocol).
- Far infrared sauna.
- Mild hyperbaric oxygen therapy (HBOT).
- Red light therapy/low-level laser.
- Normatec compression equipment.
Just as we can pick and choose which motion analysis protocols we use for each individual athlete, we can also pick and choose which recovery methods we use, based on individual needs identified on assessment. All of the recovery techniques described are done in a gravity-eliminated position (on a massage table or supported sitting). This decreases external load on the body from gravity and is “safe” for the nervous system since it is how we first learn to move as infants.
I would start this client with passive recovery methods (for example, sauna, red light therapy, myofascial release). After several sessions, I would move toward more movement-based recovery, primarily movement re-patterning (MNRI techniques), still in the gravity-eliminated position. These techniques progress the client through foundational movement patterns starting passively, progressing to isometric, and then to isotonic when the client shows readiness.
Once this client presents with less systemic stress and better foundational movement patterns, I would progress her program to integrate corrective exercise techniques (upright/against gravity), starting with isometrics and progressing to isotonic exercise. We would then strategically increase loading within the corrective exercise phase while continuing to incorporate recovery methods, likely with less intensity and frequency. The strategic application of dense recovery methodology in the initial phases of rehab establishes a strong foundation for this client to be able to move from distress to eustress, returning to baseline and adapting beyond it on the SRA graph.
The strategic application of dense recovery methodology in the initial phases of rehab establishes a strong foundation for this client to be able to move from distress to eustress. Share on XIt is important to periodically reassess movement quality, especially for the rehab client. In this client’s case, I will reassess postoperatively and once a month after that to monitor progress and individual response to programming.
Let’s look at another data set from a performance-based athlete.
Case Study 2: Performance-Based Athlete
The next data we will look at is from a healthy athlete in his late 20s. He is a personal trainer and follows a pretty intense (5-7 days/week) training regimen. He describes his training style as “heavy strength and conditioning,” focused on improving performance and athletic development. This athlete is also very active outside of the gym, with activities such as biking and rock climbing. His injury history is significant, with a right shoulder injury requiring surgical repair, right foot fracture, right knee injury, and possible labral tear in the right hip.
The athlete wanted to use motion analysis to look at neuromuscular symmetry within his squat. The EMG arrangement for the squat protocol is as follows (right and left side electrode placement): rectus femoris, biceps femoris caput longum, rectus abdominis, latissimus dorsi, gluteus maximus. In addition to the squat analysis, I also did a gait analysis to get information about pelvic kinematics. I chose to do the G-Walk protocol for the gait assessment, which uses only one inertia sensor at the level of the pelvis for spatiotemporal kinematics within the gait cycle.
The gait assessment using the G-Walk does not assess neuromuscular activation. The pelvic kinematics analyzed with this protocol are the same as discussed with the previous client. The pelvic data gives a good picture of multiplanar orientation of the pelvis, which is beneficial for planning targeted fascia release within the recovery aspect of treatment. I find it beneficial to correlate the data from these two protocols (gait and squat) to get the most detailed picture of the athlete’s baseline related to posture and motor control.
I find it beneficial to correlate the data from the gait and squat protocols to get the most detailed picture of the athlete’s baseline related to posture and motor control. Share on XData Analysis
Pelvic kinematics within the gait analysis reveal several deviations outside of the normative data. In the top graph, which looks at anterior/posterior tilt throughout the gait cycle, we see about 20 degrees of anterior tilt throughout the gait cycle. This is about 10 degrees more anterior tilt compared to the normative data. In the second graph, we also see significant deviation from normative data for left and right pelvic obliquity. The graph basically shows elevation of the left side of the pelvis (approximately 10 degrees) and depression of the right side of the pelvis (approximately 10 degrees). This is maintained throughout the gait cycle.
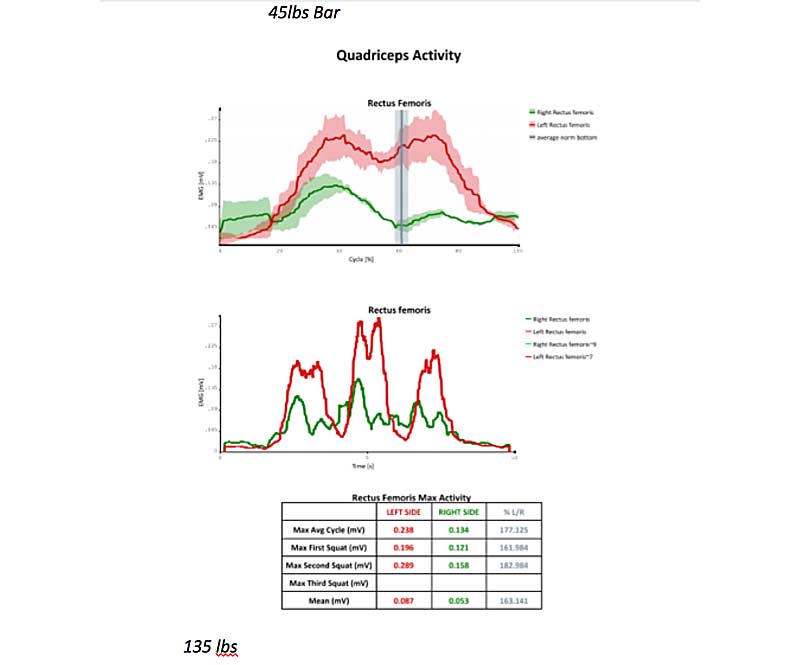
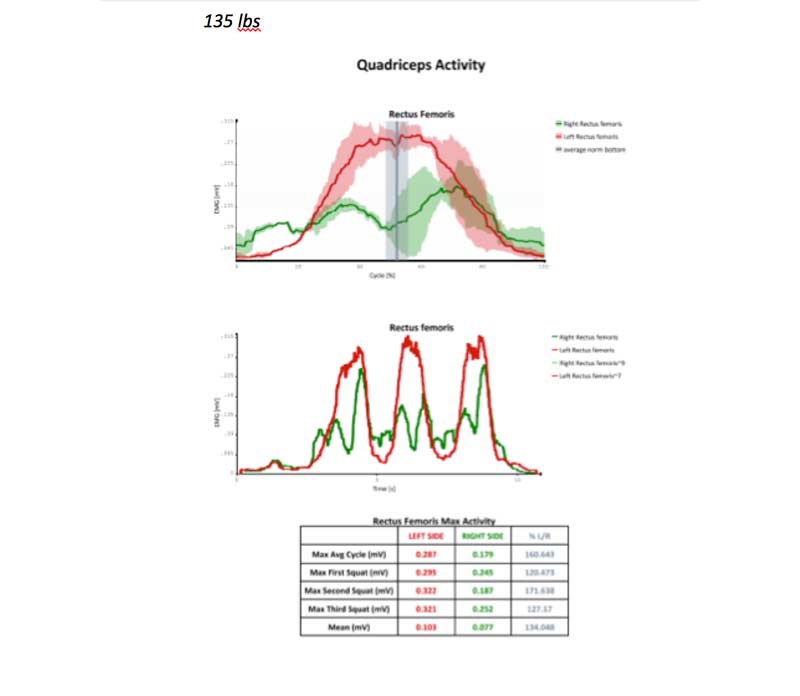
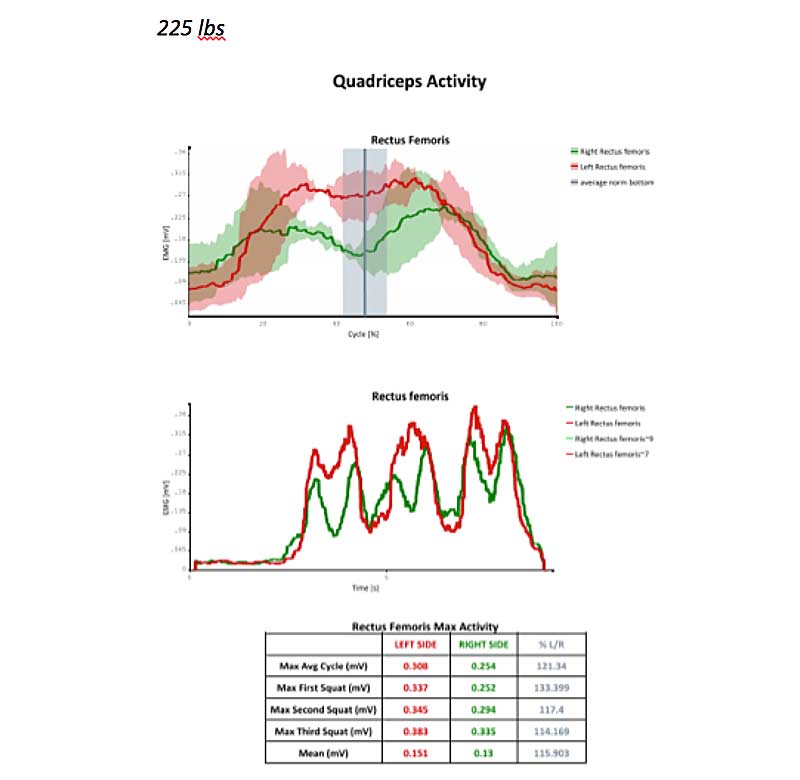
Moving on to neuromuscular analysis of the athlete’s squat technique, we did trials using bar weight (45 pounds), 135 pounds, and 225 pounds. The goal of our data collection was to identify muscle imbalances within the squat, as well as the most optimal load to re-pattern these imbalances to promote positive neuromuscular adaptations within the movement pattern.
The two muscle groups that showed the greatest asymmetry during the squat cycle were the quads (rectus femoris) and gluteus maximus.
See the data below for neuromuscular activation of the rectus femoris. Green represents the right RF, red represents the left RF, and the gray vertical line represents the bottom of the squat. The top graph is the data for all three squat reps, and the bottom graph is data for each of the trials individually over time.
This client’s left rectus femoris consistently had higher EMG activity compared to the right. The greatest asymmetry was with bar weight (45 pounds), while the most symmetrical activation was at 225 pounds. This is typical with athletes who are consistent lifters, to see better symmetry at higher loads. Their proprioceptive systems become accustomed to being loaded, and they have better body awareness under loads.
It is typical for athletes who lift consistently to see better symmetry at higher loads. Their proprioceptive systems become used to being loaded & they have better body awareness under loads. Share on XBased on the data, when we work on re-patterning this muscle group for this client, we would choose a load somewhere between 135 pounds and 225 pounds. For re-patterning, I recommend starting with a load where the athlete’s RPE is around a 4, and then progressing through loads of 5-7 RPE. We want enough weight to activate optimal proprioception; however, we don’t want them to struggle under the weight. The struggle (stress) for re-patterning should be in maintaining the mind-body connection of the targeted muscle group throughout the squat cycle.
Now let’s look at data from the gluteus maximus at 45 pounds, 135 pounds, and 225 pounds. Just like we saw in this client’s quadriceps, he shows higher neuromuscular activation in all trials and all weights in the left glute compared to the right. However, the client showed the most symmetrical neuromuscular activity with the 135-pound load. We would likely work on re-patterning this muscle group at or around 135 pounds, depending on RPE.
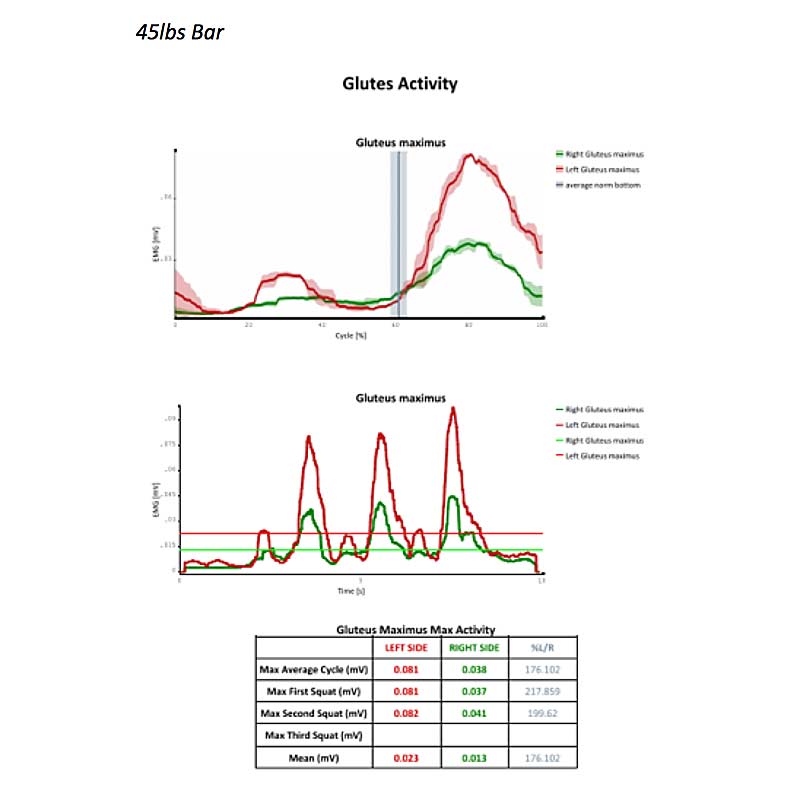
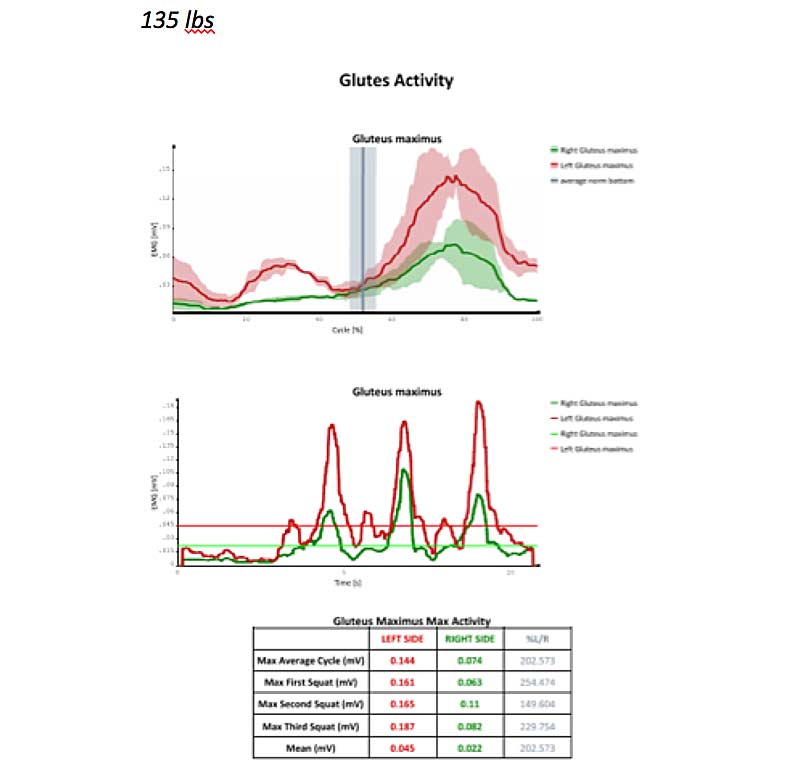
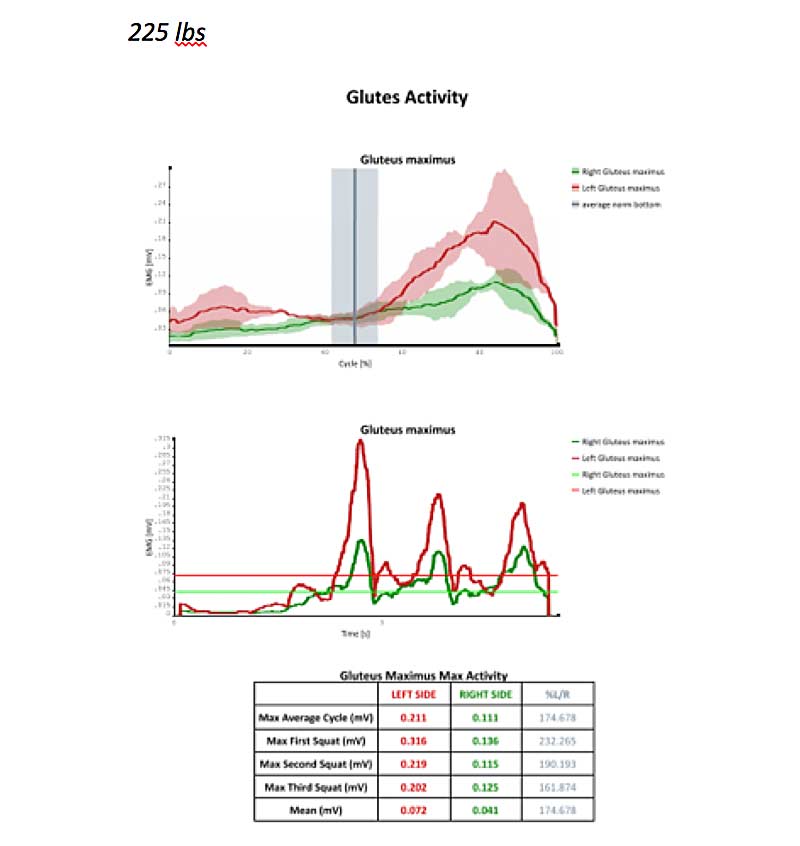
Figure 9. Gluteus maximus activity at 45 pounds, 135 pounds, and 225 pounds.
Interpretation of Results/Programming Notes
For this client’s programming, I would prioritize working on improving the position of the pelvis and re-patterning muscle activation of the quadriceps femoris and gluteus maximus in the squat. This client presents overall with much less systemic stress than the first client. I would still prioritize recovery initially with this client—primarily fascia release around the pelvis and re-patterning (gravity-eliminated position) of the core and lower extremities. However, his recovery phase would be much shorter prior to moving on to corrective exercise programming. As with the previous client, I would incorporate recovery at a lesser intensity and frequency once moving on to corrective exercise.
Biofeedback techniques that strengthen the mind-body connection, or awareness of muscle activity, are an effective means to create more functional movement patterns. Share on XThe goal of corrective exercise programming is to replace the athlete’s dysfunctional movement patterns with more functional patterns. For this athlete, we would work to improve symmetry within the quads and glutes during the squat cycle. Biofeedback techniques that strengthen the mind-body connection, or awareness of muscle activity, are an effective means to create more functional movement patterns. We can use the BTS EMG sensors in biofeedback mode, which gives visual and auditory cues to the athlete when they deviate from targeted muscle activity range.
Proper cueing from the coach or therapist and use of a mirror are other low-tech biofeedback methods. Since this client showed higher muscle activation on the left side, I would cue them to focus on the right-side muscle group. Typically, this is a good cue to use to balance neuromuscular asymmetries.
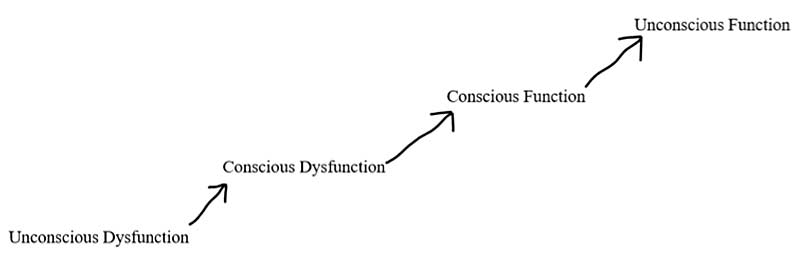
See the chart (figure 10) below for a visual of progression of how our athletes replace dysfunctional movement with functional movement using biofeedback methods. When our athletes come to us with a dysfunctional movement pattern, they are likely unaware of the specific faulty pattern (unconscious dysfunction). Through the use of motion analysis, we can bring awareness to these dysfunctional patterns (conscious dysfunction).
Using biofeedback to strengthen mind-body connection to specific muscle groups, we can consciously achieve a more functional movement pattern (conscious function). Repetition of functional movement patterns under an optimal load allows the brain to create new neural pathways, replacing the dysfunctional movement pattern with a more efficient motor pathway. This is through a process called neuroplasticity—this more efficient motor pathway then becomes the dominant pathway and the athlete’s new baseline (unconscious function).
In order to establish that our programming is facilitating the positive adaptations we are targeting, we would complete repeat assessments at various intervals. For this athlete, I’d recommend a reassessment in two to three months to give the body enough time to adapt to programming efforts.
Conclusion
There should be no doubt that using high-tech motion analysis equipment allows professionals to develop highly individualized programming, based on the most objective data available. This has obvious benefits when working with high-performance athletes of any specialization. However, not all equipment is created equal, and this is one area where you truly pay for what you get. While lower cost motion analysis options might seem flashy and appealing, it is important to determine whether the equipment you are considering purchasing for use with your athletes has been validated and used in clinical trials.
It is important to make sure the motion analysis equipment you are considering purchasing for use with your athletes has been validated and used in clinical trials. Share on XUsing research-backed motion analysis systems, such as our BTS system, truly has the potential to revolutionize our industry while maintaining evidence-based practice ideals. It is our goal at EPC to use our equipment to set standards and push forward the boundaries of the human performance industry.
Since you’re here…
…we have a small favor to ask. More people are reading SimpliFaster than ever, and each week we bring you compelling content from coaches, sport scientists, and physiotherapists who are devoted to building better athletes. Please take a moment to share the articles on social media, engage the authors with questions and comments below, and link to articles when appropriate if you have a blog or participate on forums of related topics. — SF

