
Dr. Bruce Williams practices at the forefront of biomechanical evaluation and treatment of foot, ankle, and lower extremity conditions. For over two decades, he has harnessed the power of cutting-edge medical technologies, such as pressure mapping, to identify and treat high-pressure areas in the feet. Many patients seek Dr. Williams because he uses digital video and kinematic shoe analysis to identify and treat poor body alignment and function. He also uses digital foot scanning to specially design hyper-customized foot orthotics for shoes, providing a tremendous leap forward in the fight against lower extremity pain.
Freelap USA: The pelvis plays a role in transmitting forces and influencing recovery mechanics for lower extremity and foot function. Many therapists and coaches think foot strengthening, like core and hip training, will correct foot and ankle function. Can you explain the independent relationships seen in a foot strike (ground up) that must be considered when evaluating performance and injuries? How do anatomical structure and function interact, and what are some issues that can’t be modified easily with exercises?
Dr. Williams: There is no question that the hip and pelvic musculature, along with the core, can have a positive influence on lower extremity and foot function. Unfortunately, this only works about 50% of the time. When hip and core strengthening exercises do not deliver, the foot is usually to blame. Foot function and structure are often not understood well. Structure is just that—boney structure that cannot change without injury or surgery.
For example, if an athlete has a long first metatarsal that’s flexible in its dorsiflexion motion, there will be minimal pressures under the 1st metatarsal head and higher pressures underneath the great toe. The lack of stiffness in this part of the foot combined with the metatarsal’s length can lead to a functional restriction of the 1st metatarsal joint’s (MPJ) motion, called functional hallux limitus.
While the 1st MPJ’s range of motion may be good to excellent (dorsiflexion greater than 65 degrees), the joint will not properly dorsiflex if something is not done to assist the 1st MPJ to plantarflex at the proper time in the athlete’s gait cycle.
The athlete can try to strengthen the peroneus longus musculature and even the foot’s intrinsic muscles to potentially raise the arch of the foot. But if these don’t show a regular, repeatable increase in the pressures under the 1st MPJ, the problem will persist.
The literature shows that strengthening exercises can increase the cross-sectional area in small muscles, but no study has shown regular improvement in the pressures under the 1st MPJ with prolonged activity (running 3-5 miles). I’m not against strengthening exercises. I just want proof that it works the way therapists and coaches want it to. Until then, I’ll stick with what does work.
Often the only way to alleviate this functional and structural issue is to tape the foot or use a custom or customized foot orthotic. Testing with pressure mapping has shown regular benefits and improvement in the pressures sub 1st MPJ by taping and orthotic modification.
Freelap USA: Many coaches and athletes are uncomfortable with orthotics and don’t consider shoe design a factor in injuries. Barefoot running has calmed down since injury patterns like stress fractures have forced a moderation of approach. Can you share how cleat design and surfaces can increase various injuries in football and soccer?
Dr. Williams: I’ve written a chapter for an upcoming book specifically about this subject and US Football. The surface area of cleats has a huge influence on knee, ankle, and foot injuries. It’s now common to see multiple athletes injured and out for the season, or most of it, because of non-contact injuries from pre-season training and games.
Shoe stiffness greatly effects pivoting motions for players and can keep the best off the field. Share on XThe type of cleats used can have a huge effect on pivoting motions for receivers and defensive backs. This can lead to torque at the knee and ankle that can end a season or a career. Plantar placement of cleats, for example, and the segmental rigidity of shoes can influence the pressures under the 5th metatarsal.

Most professional athletes have a significant restriction in their ankle dorsiflexion range of motion which causes the heel of the foot to rise early and for a prolonged time. This increases the opportunity for cleats to stop foot rotation in relation to the knee and ankle and increase pressures under the fifth metatarsal, leading to huge risks.
This year, a video showed a player’s Achilles tendon rupturing as he battled another player while blocking. You could see his shoes dig into the turf and the unfortunate rotation of his foot to his leg and how this increased his risk of injury. Shoe stiffness and cleats are big barriers to keeping the best players on the field. It is unfortunate that the NFL is not doing more to look into this scientifically.
Freelap USA: You have a special evaluation system to connect very complicated joint systems to pressure mapping. Can you tell us how one can learn to evaluate the foot and ankle complex, ranging from simple things a coach can do to more sophisticated actions physical therapists and podiatrists can take?
Dr. Williams: It’s imperative to complete a comprehensive foot and ankle evaluation when using and interpreting pressure mapping data output. The foot and ankle have very specific functional and structural segments that contribute to overall foot function during gait.
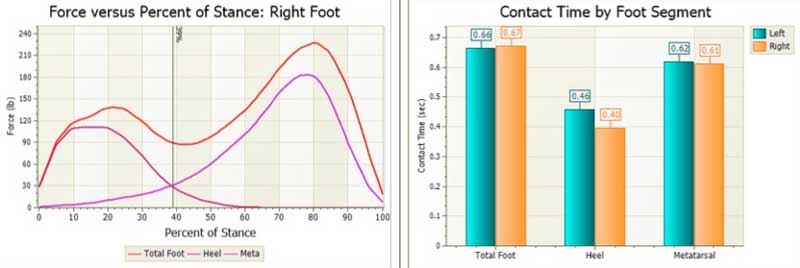
If you don’t have this basic evaluation data, then you won’t be able to fully appreciate what pressure mapping data means and how best to improve upon foot and ankle function. It’s one thing to notice a high-pressure area of the foot with pressure mapping; it’s something entirely different to understand the foot’s underlying function and know why and when that high-pressure area occurs.

My evaluation system is the Mercury XML. It’s a segmental foot and ankle evaluation tool that will echo pressure-mapping output about 80% of the time. It is repeatable and teachable to any practitioner. It’s simple and takes about ten minutes with practice. The system is taught online via Skype or in-person and on site for universities and teams. Video tutorials are available as well.
Freelap USA: With pressure mapping, what are the differences between in-shoe pressure and some of the wearable devices like Runscribe and the IMU (inertial measuring units) tibial device? Many sports teams want wearable systems for data but don’t understand how some metrics are not actionable.
Dr. Williams: In-shoe pressure systems use sensors that fit into an athlete’s shoes. Most of these are somewhat wireless; they’re not tethered to a computer. But most of them still have cables running down the legs attached to shoe sensors and up to a belt holding a data logging system. There’s at least one new pressure mapping sensor on the market that is 100% wireless with no belts or cables. All of these systems have varying degrees of speed with which they gather data, measured in hertz. In general, the higher the hertz, the more data you can gather per second.
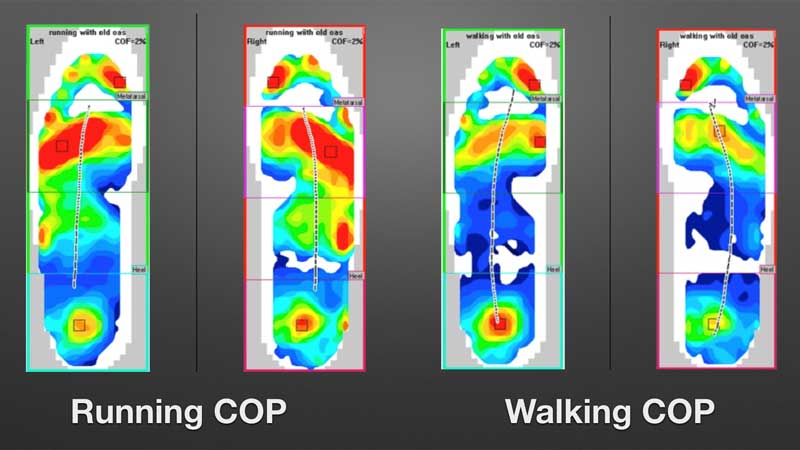
The number of sensels per foot sensor is also important. We all expect HDTV output in our images, but many of the newer systems don’t have the same number of sensels in their foot sensors as some older systems, so the data points are significantly fewer and less granular.
IMU devices are great for gathering positional and rotational data at different leg and foot segments. They are getting smaller all the time; most are now the size of a car key fob. Their data output is said to be within 80-90% of some of the best video capture hardware and software available in university gait analysis labs. Some, like Runscribe, can attach to the back of the shoe and provide pronation velocity and maximum pronation along with other information. These are great contributory tools for getting the most data you can about athletic movement.
While many teams are using these devices now, I think they’ll quickly realize the systems provide very little actionable data regarding foot and ankle function and how these segments affect overall athletic gait.
“Inertial measuring units combined with pressure mapping provide significantly more actionable data of foot and ankle function.”
Combined with pressure mapping, IMU’s can provide significantly more actionable data. Without pressure mapping, the data will not provide enough information to know where, what, and how to approach the roles of the foot and ankle in athletic movement.
Freelap USA: Finally, will you explain the pros and cons of 3-D printing and other orthotic fabrication processes? Many of the scanning systems used to create athletic orthotic devices skip the clinical side of the process, and this could spell disaster for an athlete.
Dr. Williams: Orthotic fabrication is a special pet peeve of mine. There are many ways to create orthotic devices. CAD/CAM systems are available in labs and for in office-creation of devices. There are many types of materials for creating orthotics with many varying densities. Startup companies are now making 3-D printing available, attempting to disrupt the traditional orthotic market.
No matter what type of manufacturing process you choose, you need to do a thorough foot and ankle exam to make sure you know the important variables to affect in the foot to improve your athlete’s problems and movement patterns. The way you take a cast or scan of the foot is also very important.
Many of the startups use still pictures of the feet, or pressure mats, (either on or off weight-bearing) as the basis for their orthotic devices. Most practitioners, PT, DPM, Chiro, and others use Plaster of Paris or foam boxes for their casts or laser scans for their images for orthotic manufacture.
Any of these are appropriate when done by an experienced practitioner who knows exactly how to position the foot to maximize the orthotics function. Ultimately, the most important element is the prescription of the device itself. Regarding ankle joint restriction and other issues, most startups only provide a foot bed with no prescription elements. The Mercury XML provides an orthotic prescription to maximize the output of the orthotic device as well as prescription elements for taping.
Since you’re here…
…we have a small favor to ask. More people are reading SimpliFaster than ever, and each week we bring you compelling content from coaches, sport scientists, and physiotherapists who are devoted to building better athletes. Please take a moment to share the articles on social media, engage the authors with questions and comments below, and link to articles when appropriate if you have a blog or participate on forums of related topics. — SF


Great piece of information. Gait analysis is an excellent way to understand the common biomechanics linked with injuries. It is also an important tool to figure out if the injury is due to a musculoskeletal impairment, a training error, faulty running mechanics or extrinsic factors like footwear.
Apart from research papers, there are a number of free courses that clinicians can use to learn gait analysis.
Free Course on the biomechanical analysis of runners: https://www.youtube.com/watch?v=Cb0pwvFdlqU&t=17s