[mashshare]
It is not uncommon to go through the day and encounter a reference to “stem cell” therapy as a health-care solution, whether you are reading the newspaper, listening to radio or podcast interviews, or even having a casual conversation with friends and colleagues. Stem cells are certainly the medical “flavor of the month,” particularly with a growing aging population that desires to stay young, healthy, and active. In the realm of professional sports, stem cell therapies are attracting more and more attention for orthopedic injuries and soft-tissue strains as a means of extending professional careers and also returning athletes to the field or court of play in a shorter period of time. Regardless of what you have heard about this “technology,” stem cells are here to stay and will become a bigger part of health care, whether you are scoring touchdowns in the Super Bowl or hoping to walk your dog in the park in your retirement years.
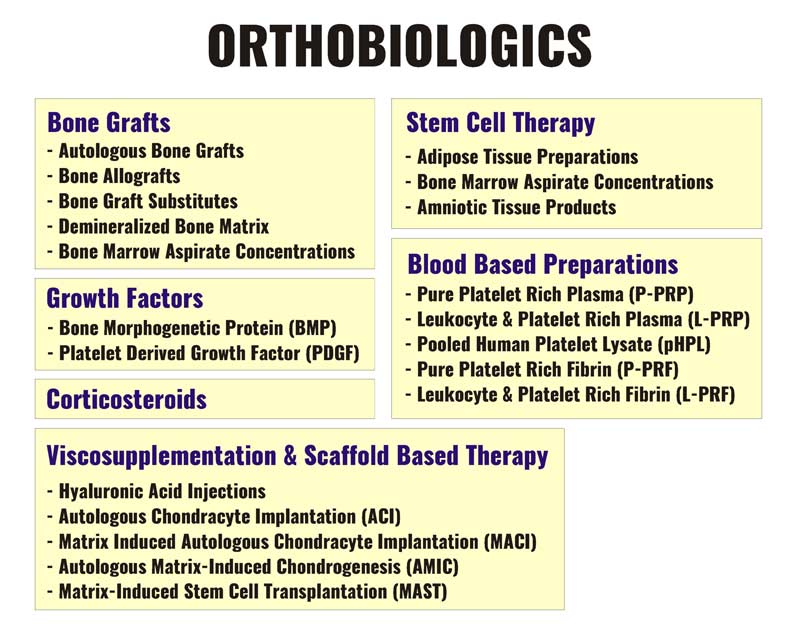
Stem cell therapies as they relate to orthopedic injuries fall under the category of orthobiologic interventions. Our clinical and practical involvement with orthobiologics spans several decades. The term “orthobiologics” refers to the use of biological substances to assist in the faster and more complete healing of musculoskeletal injuries. These substances are used to improve the healing of fractured bones and injured muscles, tendons, cartilage, and ligaments, and are obtained from substances that occur naturally in the body. When orthobiologic substances are applied in relatively high concentrations, they can potentially speed up the healing process. Common forms of orthobiological interventions include:
- Visco-supplementation products
- Corticosteroids
- Bone graft preparations
- Platelet-rich plasma (PRP) injections
- Growth factors
- Stem cell therapies
It is important to note that there is significant overlap between these interventions, as many of the compounds in these processes can involve growth factors, stem cells, and other regenerative substances. We have also seen prolotherapy injections and food supplements identified as orthobiologics and they are often deemed “regenerative” approaches. Figure 1 identifies numerous types of orthobiologic treatments being used in modern regenerative medicine. It is important to note that a universal classification method for these categories has not been adopted, and we are simply attempting to display and document these approaches for discussion purposes.
It is worth acknowledging that while many of the innovations with regard to stem cell therapies are rapidly evolving, in the realm of orthopedic injuries, very little research has been documented that supports its efficacy and sustainability in human populations. The research around conventional orthobiologic interventions, such as the use of platelet-rich plasma, has been much more robust and supportive—PRP has been in practice for many more years and is significantly less expensive than current stem cell treatments.
At the 2018 NFL Combine, we had the pleasure of viewing Dr. Brian Cole’s presentations on orthobiologic interventions in sports injuries. It was interesting to hear that while he uses stem cell therapies for various cases, he had very positive comments on his experience with, and continued use of, PRP injections, despite the trend towards embracing stem cells for regenerative medical procedures. Accordingly, Dr. Cole reported that PRP only had 20 million Google searches in 2017, while stem cells had 94.5 million. Hence, stem cells continue to be the preferred search for the modern patient despite the efficacy documented in research for PRP.
While the administration and evaluation of various orthobiologic approaches continue, there has been very little investigation into the processes that surround regenerative medicine. In particular, the specifics of the physical rehabilitation and return-to-play process associated with orthobiologics have not been identified in any great detail, but only in concept. In 2018, a study published in the Journal of Orthopedics and Trauma, by McKay et al., titled “Rehabilitation Following Regenerative Medicine Treatment for Knee Osteoarthritis – Current Concept Review” identified a conceptual rehabilitation approach following orthobiologic interventions, but only outlined a relatively general timeline for integration of individual therapies and exercises.1 One of the most significant statements made in the study was:
-
“Limitations of our study include a large portion of the studies reviewed were not done concurrently with orthobiologic intervention. There is minimal research in the field of rehabilitation of patients post orthobiologic intervention with KOA although there is significant literature in the use of regenerative medicine in patients with KOA.”
Thus, the study was essentially a review of individual therapies and interventions in isolation that were not necessarily part of an orthobiologic procedure, and not evaluated as part of a broader, organized process. A more comprehensive and integrative rehabilitation approach that identifies specific protocols (timing, volumes, frequency, intensities, durations, etc.) for various orthopedic injuries and orthobiologic interventions must be developed to help guide both physicians and physical therapy professionals through the entire regenerative medicine process.
Provided below is an outline for a process directed at providing support for the administration of orthobiologic interventions. While we are learning more and more every day about the technologies and timelines around orthobiologics, our primary efforts are focused on surrounding every aspect of the orthobiologic treatment with a supportive environment for full and active recovery of the patient. Through daily hands-on experience, we are becoming more adept at solving the problems of when, how much, and how frequently when it comes to physical therapy interventions, the use of electrical stimulation, and the introduction of voluntary exercise.
Initiating Effective Assessment Protocols and Diagnoses
One of the most eye-opening trends that we experienced while being associated with a regenerative medicine practice, particularly when stem cell therapy was advertised as a potential solution, was the high incidence of patients who simply had poor quality of previous care and substandard assessments of their true condition. Due to their less-than-fulfilling experiences with other health-care practitioners, they were attracted to the allure of new and innovative “stem cell” therapies to resolve their chronic pain and discomfort. Hence, one of the key components of a complete orthobiologics support system is initiating the process with a comprehensive evaluation of the patient to identify the true cause of their discomfort, as well as assessing the efficacy of previous diagnoses and rehabilitation efforts. Provided below are some of the more common “gaps” that we have seen in the continuum of care of new patients when reviewing their history.
Inadequate or Non-Existent Imaging
A surprising number of patients inquiring about the possibility of stem cell therapy did not have adequate imaging to support their initial diagnosis. Although they were told they might have damage or degeneration to bone, ligament, tendon, or other connective tissues, there was rarely adequate imaging to support these diagnoses. Health-care practitioners were going on “hunches” or their regular stream of treatment, rather than digging deeper into the true causes of their patients’ discomfort and dysfunction. Needless to say, one of our first recommendations for these patients was to seek a referral for appropriate and current imaging to provide a clearer “picture” of their true status.
Narrowly Focused Source Identification
When asked about their previous examinations by physicians and physical therapists, it was very common for patients to relay that the exam only focused on the specific location where they were experiencing pain. Patients with knee pain were only assessed and/or treated at the knee joint. Low back pain assessment and treatment focused only on the lumbo-sacral region. When we incorporated functional movement and postural assessments—thus taking a more comprehensive and global examination of skeletal and soft-tissue structures—clearer patterns of etiology began to emerge that assisted in both an accurate diagnosis and effective treatment planning.

No Previous Experience with Conventional Orthobiologic Interventions
While stem cell therapy appears to be the “shiny object” that attracted people to our support services, it was interesting to note that many patients had no prior knowledge of other types of orthobiologic treatments for their condition. Perhaps the name “platelet-rich plasma” was too difficult to understand, or their referring physician did not have enough information on the technology to make an informed referral for the process. Nonetheless, it became clear that patients needed much more information on the options that were available to them.
Additionally, patients needed enhanced awareness of the variability in quality of orthobiologic options from practitioner to practitioner, as well as what actually constituted a stem cell product. Many of our patients were under the assumption that PRP treatments were, in fact, stem cell therapy. The lack of education around these various treatments has only created more confusion around nonsurgical options for patients.
A general lack of clarity and regulation around the orthobiologic industry has led to poor decision-making, less-than-positive outcomes, and misleading marketing. Share on XFurthermore, in the case of PRP injections, some patients expressed disappointment with the ineffectiveness of their previous experiences with PRP, only to find out their injections were either prolotherapeutic (Dextrose) or not guided by either ultrasound or fluoroscope. A general lack of clarity and regulation around the orthobiologic industry has led to a combination of poor decision-making on the part of patients, less-than-positive outcomes for numerous procedures, and misleading marketing by unscrupulous practitioners.
Facilitating Appropriate Structural Alignment, Stability, and Mobility
While we all recognize that individual human beings can exhibit various degrees of variability when it comes to posture and movement, there are some basic truths and realities around skeletal alignment, joint stability, and overall mobility that must be followed as part of a comprehensive orthopedic rehabilitation and physical therapy process.
We know that skeletal and joint alignment can significantly influence motor control and muscle length-tension relationships through the detection of mechanical stimuli via the muscle spindles2 and golgi tendon organs.3 In addition, synovial joints are recognized as sensory organs that provide continuous feedback about position sensing and degree of limb movement.4 Misaligned joints and skeletal structures have significant implications for movement efficiency, human performance, and joint wear and tear, as well as pain and discomfort in all populations. If an individual’s skeletal structure is not aligned properly within specific relative tolerances—and stable within that operating range—neuromuscular output capabilities inclusive of power and balance will be greatly compromised. Additionally, articular cartilage, menisci, joint capsules, ligaments, and tendons will continue to be unduly stressed and micro-traumatized regardless of the efficacy of the orthobiologic intervention applied prior to rehabilitation, due to the nature of unbalanced forces across the joint.
-
“Injuries and disorders that directly damage the joint structure or lead to joint instability are highly associated with osteoarthritis (OA).”5
As such, it is imperative to ensure the skeletal structures and joints are optimally aligned both prior to and following an orthobiologic intervention. It is no different than adjusting wheel alignment following the installation of new tires on a high-performance motor vehicle. This is done to ensure maximum traction and stability at high speeds, as well as manage appropriate and even wear of the tires for safety and longevity. Cars and humans share many of the same requirements for both healthy and safe locomotion, particularly at high levels of performance.
Cars and humans share many of the same requirements for both healthy and safe locomotion, particularly at high levels of performance. Share on XEnsuring for appropriate ranges of motion and mobility in a joint system is also critical for managing stressors through a load-bearing system and kinetic chain. Restricted range of motion in a load-bearing joint can lead to a significant shifting of load to unaccustomed muscles and joints. We in the rehab industry commonly refer to this as “compensatory loading” and this phenomenon leads to a lot of overuse type of injuries.
-
“An injury causing inherent losses in passive tissue stiffness (specifically disc or ligament) results in joint laxity that necessitates higher levels of muscular activation/stiffness to ensure sufficient stability.”6
Both chronic and acute injuries can result from these compensational shifts created by restricted ranges of motion. Following orthobiologic interventions, the gradual but deliberate achievement of full ranges of motion is critical to the successful outcomes where efficient and effective output is required by the patient during movement.
Implementing Adequate, Timely, and Progressive Loading
Once the primary physical therapist determines that a patient is exhibiting appropriate measurables in the realm of alignment, stability, and mobility, the next phase in the progression of care is the “loading” phase. Within the realms of rehabilitation and physical training, we often hear the term “loading” used to describe the volume and intensity of work being done by a patient or athlete. In many cases, the obvious definition of “loading” for the layperson is using some form of external resistance or weights to load an individual.
While conventional resistance training can be part of the progression, we must recognize that there is a specificity to loading that must be embraced throughout the process. Much of this specificity relates to the individual circumstances of each patient, including previous volumes and levels of function prior to the orthobiologic intervention, as well as expected function following completion of the rehabilitation process.
If a 20-year-old competitive male swimmer is being admitted for an orthobiologic procedure for a shoulder injury and has accumulated a significant training history prior to the appointment, his loading progression following the procedure will look significantly different than a 60-year-old female shoulder patient with little or no formal physical training in her history. Add into the mix the fact that the 20-year-old swimmer wants to be ready for the Olympic trials in eight months, and we have an even more ambitious progression of work.

It is imperative that any decided-upon loading progression does not delay, impair, or spoil the work of the orthobiologic procedure. For example, once patients are discharged from a PRP injection session, they are typically provided with basic guidelines for the first 3-5 days to maximize the efficacy of the procedure.
- Abstain from taking anti-inflammatory or anti-coagulation medication such as aspirin or common nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen, naproxen, or Celebrex.
- Immobilize the joint with a brace or sling to prevent disruptions to the treated tissues.
- Avoid any strenuous exercise or lifting.
- Keep the injection site clean and dry to avoid infection.
However, beyond these general guidelines, it is extremely difficult to find any specific information on types of exercises and densities (volume, intensity, frequency) of loading for different populations for the broad range of orthobiologic procedures available to patients. When it comes to exercise, we have heard of physicians restricting patients from exercise for as long as 3-4 weeks, if not longer. Much of this can be chalked up to a lack of knowledge on the part of physicians around progressive exercise and a tendency to back off and opt for the most conservative approach. However, this extremely risk-averse approach can lead to protracted healing times and unsatisfactory results on the part of the patient.
When physicians restrict patients from exercise for weeks after a PRP injection, it can lead to protracted healing times and unsatisfactory results. Share on XIn a recent case that involved a PRP injection in the sacroiliac joint area, one of our patients complained about excessive stiffness and a lack of mobility through the region, accompanied by some soreness 3-4 weeks following the procedure. When we questioned her about her exercise activity during this period, she said that she was told to do very little, with the exception of walking and stretching. This individual was previously very active and a regular gym user. It was clear to us that her lack of resistance training for the last month was contributing to her stiffness and, to some degree, atrophy of certain muscle groups in and around the treatment site. As such, our immediate recommendation was to get back into a regular exercise schedule with some specific guidelines around progressing gradually and limiting unilateral or split-stance lower body work for the initial phase of training. Not only was our recommendation met with immediate joy, but also some significant results in a very short time.
Using the ‘Right’ Tool at the ‘Right’ Time
Practitioners in the rehabilitation realm often push their certifications in specific methods front and center or their use of a specific technology or modality as the magic solution to every patient’s ailment. Very infrequently do we hear about the process and decision-making behind the timing and implementation of various tools and toys. Within the realm of orthobiologic support, the application and timing of the tools and techniques must be exceptionally precise and well-coordinated.
Within the realm of orthobiologic support, the application and timing of the tools and techniques must be exceptionally precise and well-coordinated. Share on XOne of the modalities that we have seen enhance the entire orthobiologic support process is electrical stimulation, in various forms. In the early stages of an orthobiologic intervention, electrical muscle stimulation (EMS) can be used to manage muscle tension, minimize atrophy, enhance local and peripheral circulation, and minimize pain. Electrical stimulation has also been shown to boost the efficacy of stem cell therapy for nerve regeneration7 and influence stem cell behavior through the use of electrical fields in vivo and in vitro.8 Unlike ice and anti-inflammatory medication that may limit circulation or interfere with the healing process, electrical stimulation can facilitate the natural process of healing without introducing risk in and around the treatment site.9 Even in cases where a temporary cast, brace, or sling is required in the first week following a treatment, electrical stimulation can be safely integrated as part of the recovery and regeneration process to maintain muscle strength and improve overall outcomes.
As the patient transitions out of the early healing phase following an orthobiologic procedure, electrical stimulation can be combined with exercise (superimposed electrical stimulation) to further enhance recruitment and overcome the natural tendency for inhibition following an injury and associated orthopedic procedures.10 The use of electrical stimulation also supports the initial priorities of managing and maintaining alignment, mobility, and stability with joints during the reintroduction of high volumes and loads of exercise.
Other tools are used throughout the process to continue to manage pain and discomfort, malalignment, instability, joint restrictions, and overall output (strength, power, velocity). This may include, but is not limited to, specific soft-tissue techniques, manual therapy protocols, dry needling, IMS, proprietary ultrasound techniques, and various forms of stretching. The tools used in a session are ultimately at the discretion of the practitioner, but detailed guidelines around the use of each strategy have been identified for every injury scenario and orthobiologic procedure as part of our process. While some practitioners may have the ability to implement all of these tools at any given time, the process may necessitate a system of close cross-referrals to ensure that the patient is getting the best treatment at the right time.

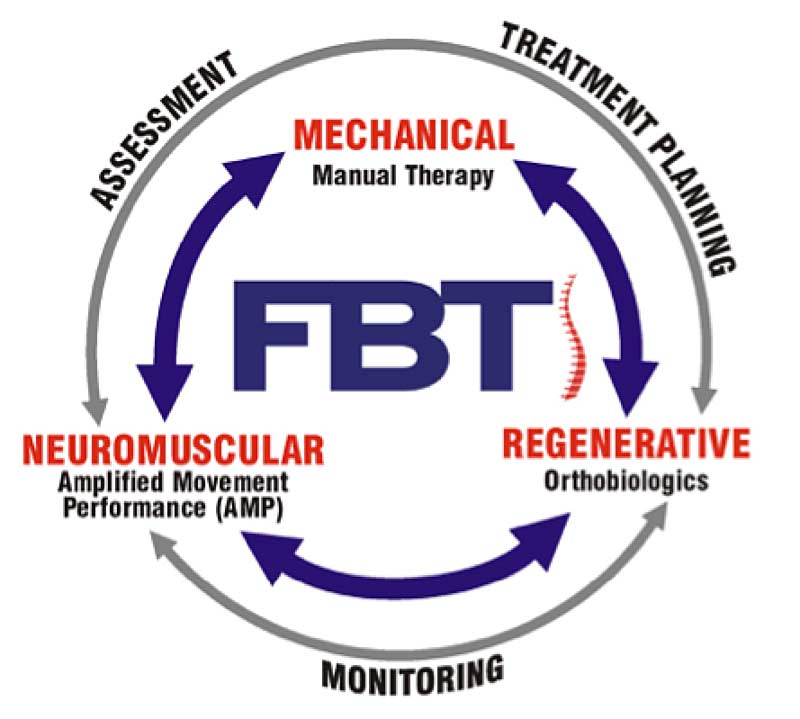
We have branded the process “Force Balance Technique” (FBT)™, as illustrated in Figure 2. Mechanical techniques are closely integrated with neuromuscular loading strategies to effectively treat chronic injury and safely support the regenerative qualities of orthobiologics, if needed. A typical session involves the close interaction of mechanical interventions—i.e., massage, joint mobilization, IMS, acupuncture, fascial release, etc.—with superimposed EMS neuromuscular loading. Adjustments on a table may be quickly followed by a loading procedure on the gym floor to not only test the intervention, but also quickly solidify a desired movement pattern.
In the case of a knee or hip injury, efforts to loosen overactive musculature in the lower kinetic chain through dry needling can be followed immediately by an appropriate loading in a squatting or deadlift exercise to evaluate strength through a given range of motion, as well as determine if pain is still present during a loaded scenario. For soft-tissue injuries in a running athlete, we often place the athlete in an acceleration or upright running activity following a minor adjustment on the treatment table to monitor gait characteristics at various velocities. This process could have the athlete moving back and forth over several repetitions until the right “balance” of mechanical and neuromuscular loading is achieved for that particular session. We commonly refer to this interplay as “hardware and software upgrades” when discussing it with patients.
Throughout the entire session and process, patient data and measurables are constantly being collected and reviewed, with video assessments performed for every movement to capture movement in action for the patient’s electronic records. Team members can review this information at any time during the process to evaluate patient progress.
The ‘Art’ of Orthobiologic Support – Knowing When to ‘Push’ and When to ‘Pull Back’
It is not uncommon for patients referred to us following orthobiologic intervention to have questions about why their procedure has not yet resulted in an improvement. The typical clinical expectation is that we will see reduction in pain and improvement in function within 4-8 weeks, although this is dependent on the composition of the injection and the structure(s) involved.
We typically see a reduction in pain and improvement in function within 4-8 weeks, although this is dependent on the composition of the injection and the structure(s) involved. Share on XOften, upon further examination, we find that the practitioner who conducted the orthobiologic procedure has either advised the client to do nothing or simply not given them any specifics on loading or stretching principles to assist in healing. As a result, it is not uncommon to see patients with moderate functional deficit and pain due to malalignment and/or mobility issues that were not addressed properly pre-procedure.
The typical example is a medial compartment of the knee pathology (meniscal tear, OA) injected in the presence of a moderate ankle pronation and/or ipsilateral pelvic rotation left unbalanced. As we mentioned earlier in this article, this logic and/or careless attention to detail is one common and easily remedied factor that leads to poor regenerative outcomes and, ultimately, frustration and great expense for the patient.
While we understand that exceptional care and due diligence are required during the early stages following application of orthobiologics to maximize efficacy, placing appropriate stress on the patient in a timely fashion is also required to create positive adaptations and facilitate healing.
Exercising the “art” of orthobiologic support requires strong and frequent communication between all practitioners. We have both “mechanical” and “neuromuscular” practitioners working in the same room with patients, interacting during a treatment session to identify opportunities for strengthening the patient while at the same time establishing boundaries around specific ranges of motion, velocities, and loads. In some cases, additional imaging may be required to validate a diagnosis or give practitioners confidence that the correct path has been chosen in treatment planning. However, moving a patient from left to right along our treatment continuum is an objective in every session. If one step backward has to be performed in order to ultimately move the patient 2-3 steps forward and beyond, all team members are consulted on the decision.
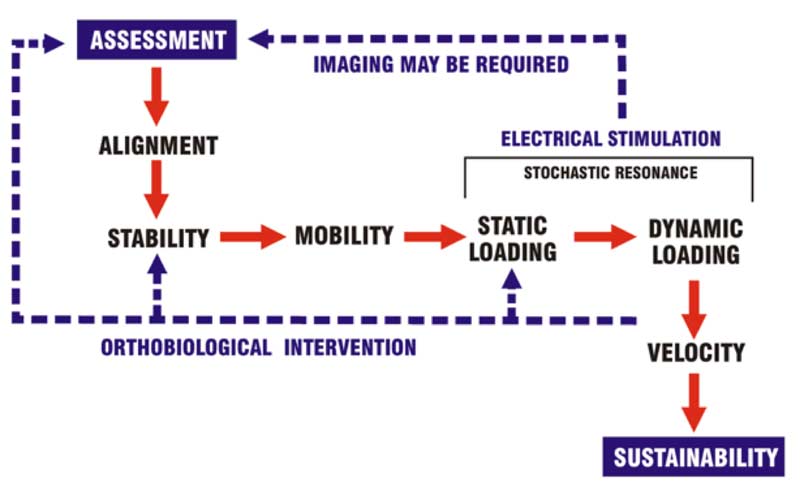
Figure 3 illustrates the conceptual flow of the process around orthobiologic support and “Force Balance Technique.” While it is convenient to depict the process in a relatively linear fashion, the reality is that the process can sometimes be fraught with roadblocks, challenges, chaotic events, and spontaneous decision-making on the spot. The two factors that almost always guide us along the correct path are “experience” and “communication” by team members.
There will not always be research papers and user manuals to guide you through a process that is rarely black and white. The teams that can navigate successfully through the gray areas of health care and rehabilitation will always have much more success than those that do not have the same levels of experience and communication. While many physical therapy practices claim to operate under a multidisciplinary approach, very few effectively integrate expertise under one roof and operate in the interdisciplinary fashion required for successful orthobiologic outcomes.
The Process Moving Forward
When we recently outlined our orthobiologic support algorithm in a formal presentation to a group of local physicians, they were extremely happy to have the ability to refer nonsurgical patients to a well-organized approach to rehabilitative care. One of the doctors even said, “This is great… But shouldn’t all physical rehabilitation occur within the integrative model that you have just outlined? It just makes sense!” Our reply was, “…well, yes.”
Unfortunately, we had to remind the doctor how fractured the current system is, with many disciplines competing with one another rather than finding common ground and supporting each other for optimal results. Although many view orthobiological innovations as the panacea of nonsurgical regenerative treatment, we must be careful to pay special attention to the entire process around patient care. A quick- fix, shotgun approach will only result in recurring orthopedic problems that will inevitably end in more invasive surgical procedures.
Our intent is to educate practitioners and patients on the need for a systematized approach to rehab inclusive of orthobiologic intervention when appropriate and necessary. Share on XOur intent moving forward is to educate both practitioners and patients on the necessity of a systematized approach to rehabilitation inclusive of orthobiologic intervention when appropriate and necessary. Unfortunately, proper source identification via thorough assessment and treatment planning are not the rule, and work has to be done to articulate the minimum steps necessary to ensure rehabilitative and regenerative efficacy.
Once we all understand the importance of a progressive and integrative approach, consistent results will be achieved in a timely manner. In a time when instant gratification is attained through personal technology hundreds of times per day, the necessary steps must be taken to gradually support the relatively new orthobiologic technologies available to individuals. Knowledge will ultimately be the most valuable technology that we can offer.
Since you’re here…
…we have a small favor to ask. More people are reading SimpliFaster than ever, and each week we bring you compelling content from coaches, sport scientists, and physiotherapists who are devoted to building better athletes. Please take a moment to share the articles on social media, engage the authors with questions and comments below, and link to articles when appropriate if you have a blog or participate on forums of related topics. — SF
[mashshare]
References
1. McKay J., Frantzen K., Vercruyssen N., Hafsi K., Opitz T., Davis A., and Murrell W. “Rehabilitation following a regenerative medicine treatment for knee osteoarthritis–current concept review.” Journal of Clinical Orthopaedics and Trauma. 2019; 10: 59-66.
2. Bewick G.S. and Banks R.W. “Mechanotransduction in the muscle spindle.” European Journal of Physiology. 2015; 467(1): 175-190.
3. Jami, L. “Golgi Tendon Organs in Mammalian Skeletal Muscle: Functional Properties and Central Actions.” Physiological Reviews. 1992; 72: 623-666.
4. Chen C.C. and Wong C.W. “Neurosensory mechanotransduction through acid-sensing ion channels.” Journal of Cellular and Molecular Medicine. 2013; 17: 337-349.
5. Blalock D., Miller A., Tilley M. and Wang J. “Joint Instability and Osteoarthritis.” Clinical Medical Insights into Arthritis and Musculoskeletal Disorders. 2015; 8: 15-23.
6. McGill S.M. and Cholewicki J. “Biomechanical Basis for Stability: An Explanation to Enhance Clinical Utility.” Journal of Orthopaedic and Sports Physical Therapy. 2011; 31: 96-100.
7. Du J., Zhen G., Chen H., Zhang S., Qing L., Yang X., Lee G., Mao, H.Q. and Jia X. “Optimal electrical stimulation boosts stem cell therapy in nerve regeneration.” Biomaterials. 2018; 181: 347-359.
8. Tang M., Yan X., Tang Q., Guo R., Da P. and Li D. “Potential Application of Electrical Stimulation in Stem Cell-Based Treatment against Hearing Loss.” Neural Plasticity. 2018: 1-6.
9. Yamabata S., Shiraishi H., Munechika M., Fukushima H., Fukuoka Y., Hojo T., Shirayama T., Horii M., Matoba S. and Kubo T. “Effects of electrical stimulation therapy on the blood flow in chronic critical limb ischemia patients following regenerative therapy.” SAGE Open Medicine. 2016; 4: 1-10.
10. Paillard T., Margness E., Maitre J., Chaubet V., Francois Y., Jully J.L., Gonzalez G. and Borel L. “Electrical stimulation superimposed onto voluntary muscular contraction reduces deterioration of both postural control and quadriceps femoris muscle strength.” Neuroscience. 2010; 165: 1471-1475.
 Dean Kotopski, BScPT, RMT, CAc/IMS, MCPA, is the Clinical Director of Performax Health Group in Burnaby, British Columbia. Dean is a 30-year veteran of physical rehabilitation, with certifications in physiotherapy, massage therapy, acupuncture, and IMS. Dean began his professional career as an auto mechanic at the age of 18, with a passion for movement and all things mechanical. His enjoyment of athletics and academics soon led him to pursue a career in physical rehabilitation. He has significant experience supporting numerous regenerative therapies including PRP and stem cells of all derivation, and he developed “Force Balance Techniqueä,” a process around physical rehabilitation and orthobiologic support, over the past 10 years. His clients range from general population patients to world-leading professional athletes. For more information on Dean, please visit: www.PerformaxHealthGroup.com
Dean Kotopski, BScPT, RMT, CAc/IMS, MCPA, is the Clinical Director of Performax Health Group in Burnaby, British Columbia. Dean is a 30-year veteran of physical rehabilitation, with certifications in physiotherapy, massage therapy, acupuncture, and IMS. Dean began his professional career as an auto mechanic at the age of 18, with a passion for movement and all things mechanical. His enjoyment of athletics and academics soon led him to pursue a career in physical rehabilitation. He has significant experience supporting numerous regenerative therapies including PRP and stem cells of all derivation, and he developed “Force Balance Techniqueä,” a process around physical rehabilitation and orthobiologic support, over the past 10 years. His clients range from general population patients to world-leading professional athletes. For more information on Dean, please visit: www.PerformaxHealthGroup.com




