Kinesiophobia. It’s an unfamiliar term for many strength and conditioning (S&C) professionals and sports coaches. With specific regard to the postoperative anterior cruciate ligament reconstruction (ACLR) knee athlete—the focus of this dialogue—kinesiophobia is a possible significant phenomena of injury and/or surgery prohibiting an athlete’s return to their previous level of athletic performance, if they return to their sport of participation at all.
Kinesiophobia is a possible significant phenomena of injury and/or surgery prohibiting an athlete’s return to their previous level of athletic performance. Share on XKinesiophobia is an athlete’s fear that they will cause pain and/or reinjury to their injured or postoperative body part, resulting in compromised physical performance during physical rehabilitation, athletic performance enhancement training, and/or game day competition. How serious is kinesiophobia in the athletic ACLR population? It is reported that, of the more than 200,000 ACL reconstructions that occur annually in the United States, 20-50% will not return to the same sport of participation after surgery and 10-70% of those who return to sports participation will do so at a substandard level of performance.1,2
Other investigators with an in-depth meta-analysis on this subject have reported only a 47% return to previous levels of sport participation several years after primary ACLR.3 It has also been reported that younger athletes (under the age of 20) who experienced a second ACL injury also had lower “psychological readiness” measured at 12 months after ACLR.4The onset of kinesiophobia has been shown to occur early during the rehabilitation process (the initial 4-8 weeks) and has been reported to have a high rate of prevalence (61%) in the athletic ACLR population.5
It is apparent that kinesiophobia has a significant influence on the athlete’s demonstrated physical performance during rehabilitation, athletic enhancement performance training, and return to sport competition. If not prevented and presented by the athlete, efforts must be made to resolve this condition during the physical rehabilitation or training process to ensure an optimal (previous physical performance) return to athletic competition. This blog post will provide recommendations for early in the physical rehabilitation process, as well as during the athlete’s performance enhancement training, to help avoid—or, once detected, eliminate—this prohibitive phenomenon of athletic performance.
The Healing Continuum of Soft Tissue
To prevent the onset of kinesiophobia or resolve this condition once it presents itself, the athlete must re-establish the confidence to load the ACLR extremity via the application of appropriate high levels of force into the ground surface area, as well as tolerate the reactive forces from the ground surface area without the fear of knee pain or reinjury. The ability to safely stress the ACLR extremity requires a progression of applied intensity to take place.
To succeed in this, rehabilitation and S&C professionals should have an appreciation of the soft tissue biological healing process. Soft tissue healing occurs at predictable time intervals (Figure 1). As the clock may only be turned ahead for an hour annually, human biology cannot be rushed. Appropriately planned and programmed design for the enhancement of the physical qualities necessary for optimal athletic performance should be implemented at the specific time intervals that align with this healing process.
There are three stages of the soft tissue healing continuum.6,7 For the purpose of this discussion, I have provided an amended review of these stages.
- The Reaction Stage – An inflammatory stage that occurs within the first 72 hours of trauma. Characteristics of this stage include cell death, effusion, ecchymosis, and pain. These components of noxious stimuli result in a reflex inhibition and lead to muscle atrophy and a loss of strength and neuromuscular abilities (i.e., proprioception).
- The Regeneration and Repair Stage – This stage of healing occurs from 48 hours to six weeks post-trauma. During this stage of healing, fibroblasts synthesize scar tissue via the formation of type III collagen while the cellular matrix is random. This collagen or “scar tissue” is the body’s raw material for repair. It is initially laid down in a random manner, and through the various manual, prescribed exercises and treatment techniques of rehabilitation, these collagen fibers are aligned to attenuate tensile forces and stress.
- The Remodeling Stage – This stage of healing occurs from three weeks to one year post-trauma. During the remodeling stage, the body adapts to the appropriate levels of applied stress. Gradual cross-linking ensues as collagen fibers produce tight and strong scar tissue. This stage of healing is the final aggregation, orientation, and arrangement of collagen.
In review of the timelines for each stage of the soft tissue healing continuum, notice that all of these stages do not occur as individual “biological silos.” Instead, they overlap and evolve as a soft tissue healing “continuum.”
My philosophy of physical rehabilitation, as well as the eventual progression to the athlete’s post-rehabilitation performance enhancement training, is coordinated amid the soft tissue healing continuum and Hall of Fame S&C Coach Al Vermeil’s Hierarchy of Athletic Development and/or the Rehabilitation Modified Hierarchy (Figure 2). The philosophy and application of both of these hierarchies have previously been published in the scientific/medical literature8-10 as well as on the SimpliFaster site. I recommend that you familiarize yourself with both of these hierarchies in order to fully appreciate their relationship to the soft tissue healing continuum.
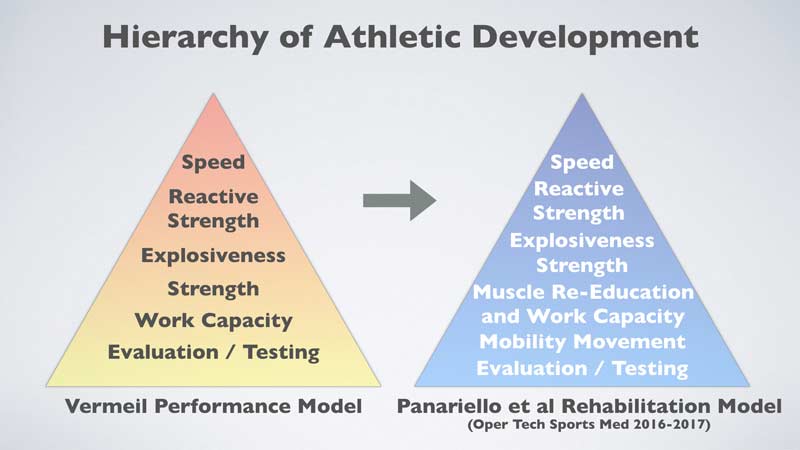
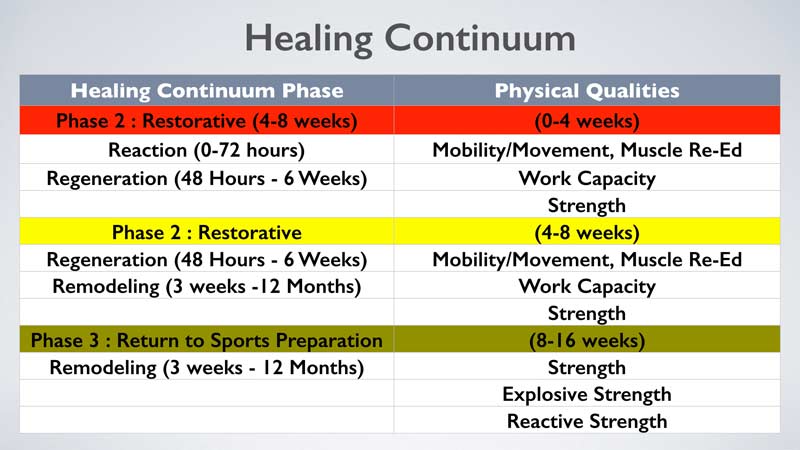
Due to the biological process of the healing continuum, the emphasis on the development of the specific physical qualities of the hierarchy should only be considered at the correlated stage of the soft tissue healing process (i.e., phase of rehabilitation). As the healing process advances, so does the level of strategically applied exercise stress (i.e., weight, velocity, etc.) that corresponds directly to the physical quality(ies) emphasized. Figure 3 presents the harmonization and timing of the soft tissue healing process in association with the Rehabilitation Modified Hierarchy.
It is important to note that the rehabilitation professional will likely not place an emphasis on the physical quality of speed during the rehabilitation process for various reasons. The focus on the development of this physical quality will likely transpire during the performance enhancement training of the post-rehabilitated athlete under the supervision of a qualified S&C and/or sport skills coach.
It is also important to note that the ACLR athlete has experienced two significant knee traumas prior to their formal introduction to postoperative physical rehabilitation. The athlete initially experiences the initial direct trauma of their knee injury (i.e., ACL tear, bone bruise, etc.), as well as other possible concomitant anatomical damage (i.e., meniscal tear, additional ligament disruption, articular cartilage damage, etc.). This initial trauma is followed by the subsequent second trauma of invasive ACL reconstructive knee surgery, including the associated requirements for this procedure to be performed safely (i.e., tourniquet time, nerve block, etc.) to repair the consequential anatomical damage caused by the injury.
Kinesiophobia can present itself early in the physical rehabilitation process.5 Therefore, the prevention of this debilitating condition should first begin during Phase I and, if necessary, Phase II of the rehabilitation process (Figure 3). The Phase I focus of rehabilitation includes the elimination of the noxious stimuli such as pain and edema, as well as the physical preparation of the athlete for the enhancement of each level of the Rehabilitation Modified Hierarchy.
Prior to the initiation of rehabilitation, communication with the team physician, surgeon, coaches, family, and athlete must occur for clarity as to the surgery to be performed, as well as the anticipated surgical outcome, awareness of any rehabilitation contraindications, and timeline of rehabilitation milestone expectations, including the athlete’s goals.
Addressing the Athlete to Prevent/Resolve Kinesiophobia
Coach Al Vermeil not only mentored and educated me on the enhancement of athletic performance, but also taught me that there are no “absolutes,” regardless of the situation. Thus, the prevention of kinesiophobia in the ACLR athlete is not guaranteed. The rehabilitation and S&C professionals must try their best to prevent and, when recognized, resolve this debilitating condition so that the athlete has the best opportunity to return to optimal athletic performance, as well as decrease the possibility of reinjury. The best period of time to prevent kinesiophobia is during the early phases (Phase I) of physical rehabilitation in order to re-establish the athlete’s confidence for the initiation of movement, the acceptance of externally applied intensity, the ability to produce force, and the ability to appropriately tolerate ground reaction forces.
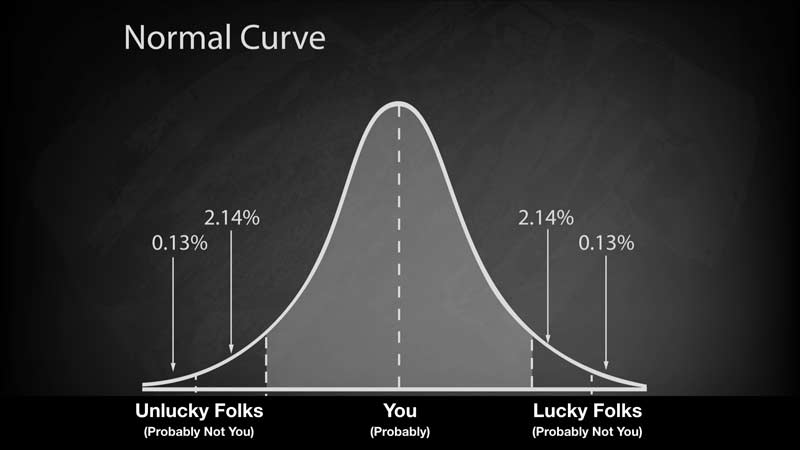
The best period of time to prevent kinesiophobia is during the early phases of physical rehabilitation. Share on XThe following is a “Reader’s Digest” version of some recommendations to implement during the initial four weeks (Phase I) of ACLR rehabilitation to prevent the onset of kinesiophobia. As all ACLR athletes are individuals, some may be able to execute these activities and adapt sooner, and others later (i.e., Phase 2), when compared to their ACLR peers. These same recommendations are also effective and may be instituted with more aggressive exercise versions in the later stages of the athlete’s physical rehabilitation as well as during the athlete’s performance enhancement training.
Movement and Mobility
During the initial phase of rehabilitation, the noxious stimuli of pain and edema, as well as quadriceps arthrogenic muscle inhibition, etc., will have an adverse effect on soft tissue and joint mobility, the athlete’s movement, the physical quality of strength (the physical quality from which all others evolve), neuromuscular mechanisms, and work capacity. These noxious stimuli, as well as any observed muscle inhibition, must be eradicated via the incorporation of modalities and manual techniques, as well as any other suitable methods and procedures utilized by the rehabilitation professional to enhance the quality of soft tissue and joint mobility, movement, and muscle function.
The re-establishment of the lower extremity musculature soft tissue compliance and joint mobility via both passive and active techniques is necessary for the progression from basic to more complex movement patterns. Basic movement patterns would include the progressions to achieve a successful gait pattern without assistive devices upon all surfaces. More complex movement pattern progressions would include advancements for the eventual active positioning of the foot/heel upon the gluteal fold (Figure 4). This foot/heel position will help to ensure proper backside swing phase mechanics at the time of the initiation of the running gait cycle.

Muscle Reeducation and Work Capacity
Due to the aforementioned traumas that happen to the athlete, the neuromuscular mechanisms of the body often “shut down,” so to speak, resulting in the aforementioned quadriceps arthrogenic muscle inhibition. The application of an external stimulus such as electric muscle stimulation (EMS) in association with the appropriate timing and application of intensity (load) will not only help to resolve this muscle inhibition, but re-establish the athlete’s ability to load (weight bear) the ACLR extremity with the confidence of the supporting lower extremity musculature.
Blood Flow Restriction (BFR) Techniques
The ability to prevent muscle atrophy, as well as to induce muscle hypertrophy and strength levels, would be of great benefit to the ACLR athlete. A larger diameter muscle fiber will produce greater levels of force as well as provide enhanced muscle and joint “stiffness.” Joint stiffness provides heightened stability at the initial phase of rehabilitation during gait training and closed kinetic chain (CKC) exercise performance, as well as during the later phases of rehabilitation, where elastic strength qualities coincide with an optimal stretch shortening cycle.
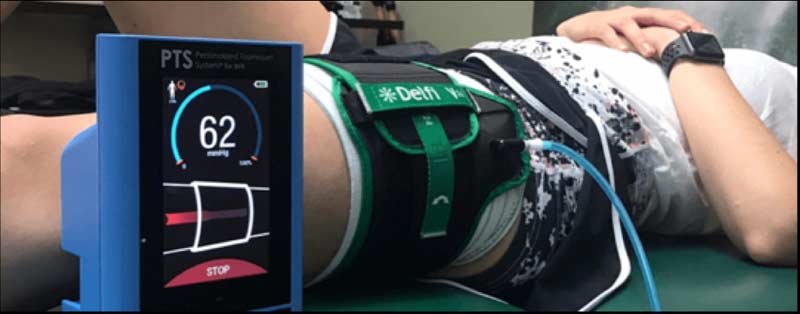
One emerging popular method in the physical rehabilitation process to prevent muscle atrophy, if not achieve muscle strength and hypertrophy, is blood flow restriction (BFR). An in-depth tutorial regarding the use of BFR is beyond the scope of this blog; however, BFR, also known as KAATSU, involves performing low-intensity resistance exercise while externally applied compression mildly restricts blood flow to active skeletal muscle (Figure 5). BFR may also be utilized in conjunction with EMS for favorable outcomes.
Acquiring muscle mass, strength, and endurance early in the rehabilitation process may help restore an athlete’s confidence in accepting load. Share on X
As BFR eases joint stress and soft tissue damage by avoiding high-intensity loads during lower extremity exercise performance (i.e., straight leg raises), it is plausible for use in the very early stages of physical rehabilitation. BFR has been noted to induce changes in muscle mass, strength, and endurance.11,12 Acquiring these physical features early in the rehabilitation process may also help to restore the athlete’s confidence in accepting load, as well as accelerate the ability to apply significant levels of muscular force.
Eliminating Weight Shift During Early-Stage Exercise Performance
It is important to initiate the execution of exercises in the standing weight-bearing (CKC) position as early and safely as possible. This is not only so stress may be applied to the lower extremity, but for the lower extremity to initiate the essential ability to react to the ground surface area as well. This is imperative for the enhancement of the physical qualities for muscle adaptation and for the adaptation of tendon (muscle-tendon complex). Restoration of the athlete’s tendon qualities includes a reliance upon ground reaction capabilities for eventual achievement of optimal elastic, reactive, and deceleration abilities. This is especially true of the ACLR athlete, for whom the autograph ligament is likely harvested from the patella, hamstring, or quadriceps tendons.
Of the various bilateral CKC exercises available for selection, we incorporate the squat exercise (pattern) early in the rehabilitation process. The choice of this particular exercise is due to, but not limited to, the following advantages:
- Bilateral exercises provide a more stable base of support, thus minimizing/eliminating the fear/concern of exercise execution.
- Many activities of daily living utilize this movement pattern (sitting in and getting out of a chair, sitting on and getting off a toilet, etc.).
- The squat pattern mimics the “athletic position” taught by sport coaches.
- Most athletic endeavors begin and end on two feet.
- Eventual greater exercise-executed intensities (loads) and initiated velocities are achieved on two feet.
- The appropriate squat pattern exercise progression will eventually lead to the achievement of a successful overhead squat pattern for optimal multiple joint mobility, soft tissue compliance, and body movement.
Initially, the athlete may express and/or demonstrate a fear of loading (weight bearing) their postoperative extremity when asked to perform a “modified” (i.e., limited depth) bodyweight squat pattern. The athlete demonstrates this apprehension by laterally shifting their body weight over the nonoperative lower extremity during the exercise execution. One method to correct this shifting pattern is to “post-up” the nonoperative extremity onto a box or surface of a specific height.10,13
The height of the box will depend upon the height of the athlete. The taller the athlete, the higher the box. When utilizing a box for the elimination of the athlete’s weight shift, a 2- to 4-inch box may initially be prescribed (Figure 6).

“Posting,” or raising, the nonoperative extremity during the execution of the bodyweight squat pattern makes it more difficult for the athlete to shift their body weight away from the ACLR lower extremity. Therefore, a greater load/stress is now applied to the ACLR extremity during the repeated exercise execution, resulting in greater muscle activity13 as well as decreased fear of loading the extremity. The athlete is continually “coached” until the time a technically proficient squat pattern is achieved with this single limb elevated upon the raised box surface. As the athlete continues to demonstrate a proper bodyweight squat pattern, the box height is continually lowered by 1-inch increments until the time when a proper bodyweight squat pattern is performed upon a level ground surface area.
The application of an exercise intensity greater than body weight is not recommended during this elevated lower-extremity squat performance. Due to this height imbalance, loading may place unwarranted stress at the sacroiliac (SI) joint, an anatomical structure where approximately 30% of all low back pain occurs. The application of an exercise intensity (load) may be prescribed at the time the athlete has demonstrated a proper squat pattern on a level ground surface at an appropriate exercise depth as determined by the rehabilitation and/or S&C professional. Exercise intensities may then be applied from the “top down” (i.e., back squat, front squat, etc.) or from the “bottom up” (i.e., trap bar deadlift, deadlift, etc.), depending upon what is best suited for the athlete.
The Isometric Mid-Thigh Pull
An additional technique in the progression of loading the post-op ACLR athlete is the incorporation of isometric mid-thigh pulls (IMTPs). This particular exercise is utilized early in the progression of exercise intensity applied in the standing bilateral position. The performance of this exercise will divert the focus of the athlete’s attention to the postoperative extremity as they attempt to “move” a barbell with a maximal effort. The IMTP exercise provides many benefits in both the rehabilitation and athletic performance training environments. The advantages of isometric exercise as well as the IMTP include, but are not limited to, reduction in pain14, as well as the testing and enhancement of strength, rate of force development (RFD), agility, and 20-meter sprint times15,16.
The performance of the IMTP will divert the athlete’s attention to the postoperative extremity as they attempt to “move” a barbell with a maximal effort. Share on XThe IMTP exercise is performed with the barbell placed in a power rack with secured steel pins or bars positioned appropriately above and below the barbell. The barbell is positioned upon the lower steel pins/bars so that the athlete’s starting exercise position occurs with the barbell placed at the mid-thigh (Figure 7).
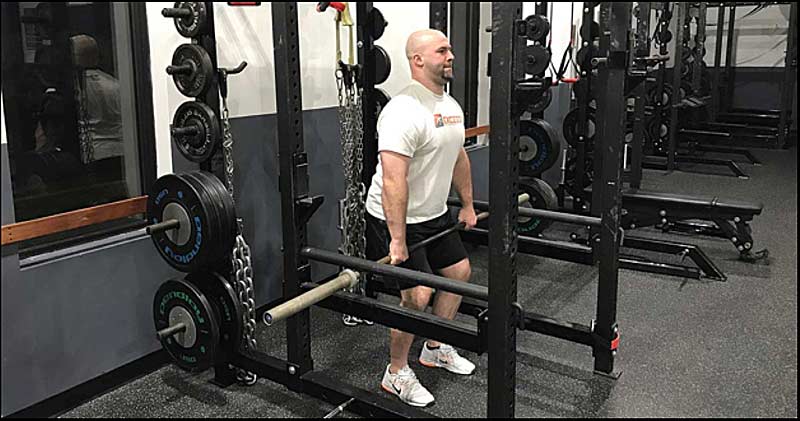
Initially the athlete will perform the IMTP submaximally to (a) become familiar with the technical exercise execution and (b) acquire the essential trust and confidence that future maximal effort isometric exercise performance will not result in knee pain or exacerbate their ACLR condition. By concentrating on maximal effort IMTP exercise performance, the concern over loading the ACLR extremity is reduced and eventually eliminated as increased levels of force are applied to the barbell via the efforts of the hip and lower extremity musculature.
Once the athlete executes the IMTP with perceived maximal effort and technical proficiency, additional weight intensity may then be added to the barbell. Weight intensity is incorporated during the IMTP so that the executed exercise efforts at least exceed the total weight of the barbell as it is raised from the lower steel pins/bars to the inferior aspect of the higher positioned steel pins/bars.
‘A’ Marches and Resisted ‘A’ Marches
Once a normal gait pattern is demonstrated without assistive devices, appropriate soft tissue compliance and joint range of motion have been achieved, and all previously noted noxious stimuli have been eliminated, the athlete may participate in low-level modified track sprint drills. During the 1950s, a Polish and Canadian track and field coach by the name of Gerard Mach developed his system of “A,” “B,” and “C” drills. In this series of track drills, Coach Mach separated the running stride into parts. These ABC drills were designed to specifically strengthen the muscles utilized in the body postures that corresponded to sprinting.
The “A” series of Mach drills were designed to work the knee lift action, which requires active hip and knee flexion, thus re-enforcing as well as improving the ACLR athlete’s lower-extremity soft tissue compliance and joint mobility. This drill advances the normal walking gait cycle via an initiated progression for enhanced lower-extremity active range of motion (AROM) in a body posture that has a correlation to sprinting (Figure 8a). Initially the ACLR athlete’s A-march drill pattern will likely be poorly performed compared to the proper drill technique. However, A-march performance, as with any exercise performance, will improve over time with repetitive practice and appropriate coaching.
The “A” series Mach drill also requires the athlete’s ACLR extremity to apply force into the ground surface area, accept ground reaction forces, and stabilize the ACLR lower extremity, as it assumes a weight-bearing role during the corresponding period of time when the nonoperative extremity is removed from the ground (Figure 8a). It is important to note that ideal A-march movement patterns are not only suitable for force production and reactivity into and from the ground surface area, but they are also a lead-up to the eventual performance of the higher velocity A-skip drill.

The A-march is progressed by externally resisting the exercise, which can be achieved easily with elastic bands. The addition of this manually controlled external resistance will now increase the athlete’s focus on overcoming the externally applied resistance and emphasize placing greater amounts of force into the ground surface area to achieve forward movement (Figure 8b). It is important to note that the manual external resistance must be increased gradually, with the athlete achieving successful initial exercise efforts. Too high a level of resistance applied too soon may exacerbate the ACLR condition, resulting in a possible loss of confidence in the ACLR extremity as well as other anatomical knee structure consequences.
The Cross-Transfer Training Effect
It has been documented that strength increases occur in the contralateral limb after exercise performance with the ipsilateral limb.17 In recent years, this cross-transfer (CT) effect has been recommended in the rehabilitation setting as a therapeutic strategy.18,19 Not only does strength training with the ipsilateral (non-involved) extremity cause an increase in strength levels, but it also results in less muscle atrophy in the contralateral (involved, non-trained) extremity.19,20Although this CT effect does provide the aforementioned benefits to muscle, there is likely minimal, if any, benefit to tendon.
In addition, as the participation of the involved (ACLR) extremity is nonexistent during the CT exercise execution, there is likely little effect on prohibiting the onset of kinesiophobia. An example would be ipsilateral exercise performance with a leg press. While the ipsilateral/non-involved extremity adapts to the stress application of the leg press exercise performance, the involved (ACLR) extremity is a non-participant during this stress application.
Utilizing this same CT muscle philosophy and methodology, wouldn’t it make more sense to perform total body bilateral standing CKC exercises early in the rehabilitation process instead of limiting the CT training effect to an isolated single contralateral lower extremity? If select exercises are performed with fully extended, “locked,” weight-bearing lower extremities, the addition of the body weight provides the ACLR athlete with the following benefits:
- Enhanced joint stability via lower-extremity knee joint agonist and antagonist muscle activity.
- Compression forces resulting in increased knee joint stability.
- Execution of exercises in the standing position, the posture of most athletic endeavors.
- The exercises are “lead up” activities, incorporating the entire musculature of the body as a segue to the athlete’s eventual advanced physical rehabilitation and performance enhancement training.
- Exercising in the standing position realizes the benefits of closed kinetic chain exercise performance.
- The athlete’s focus upon proper technical exercise performance diverts their attention from the fear of loading their ACLR extremity.
We have empirically experienced that “stiff-legged” (the athlete’s knee joints are “locked” via voluntary quadriceps isometric contraction) muscle cleans, muscle snatches, and overhead pressing (Figure 9) in the standing position not only provide the CT benefit to the ACLR athlete, but involves the entire body during the exercise performance as well. The loading of the ACLR extremity in the bilateral standing exercise posture during the exercise performance also enhances the trust and confidence of the athlete, helping to avoid the onset of kinesiophobia.
Loading the ACLR extremity in the bilateral standing exercise posture during the exercise performance enhances the confidence of the athlete, helping avoid the onset of kinesiophobia. Share on X
Final Thoughts
Kinesiophobia is a debilitative condition that not only prohibits the ACLR athlete from exhibiting their ideal physical rehabilitation and athletic performance enhancement training efforts, but it may also result in serious undesirable consequences when the athlete returns to their competitive performance. Early removal of all noxious stimuli and the re-establishment of the athlete’s strength levels, ability to confidently weight-bear, and apply and accept forces to and from the ground surface area will help prevent or resolve this postoperative ACLR condition.
It is important to take into account that all athletes are individuals and will likely present with their own particular psychological as well as physical concerns at the time of the initiation of physical rehabilitation and athletic performance enhancement training. In my experience, a sound and progressive evidenced-based program design with the associated “art of coaching” will assist to prevent or, when present, resolve the kinesiophobia that may occur in the ACLR athlete.
Since you’re here…
…we have a small favor to ask. More people are reading SimpliFaster than ever, and each week we bring you compelling content from coaches, sport scientists, and physiotherapists who are devoted to building better athletes. Please take a moment to share the articles on social media, engage the authors with questions and comments below, and link to articles when appropriate if you have a blog or participate on forums of related topics. — SF
References
1. Kvist J., Sporrsted K., and Good L. “Fear of re-injury: A hindrance for returning to sports after anterior cruciate ligament reconstruction.” Knee Surgery, Sports Traumatology, Arthroscopy. 2005;13:393–397.
2. Chmielewski T.L., Jones D., Day T., Tillman S.M., Lentz T.A., and George S.Z. “The Association of Pain and Fear of Movement/Reinjury with Function during Anterior Cruciate Ligament Reconstruction Rehabilitation,” Journal of Orthopaedic & Sports Physical Therapy. 2008;38(12):746–753.
3. Arden C.L., Webster K.E., Taylor N.F., and Feller J.A. “Return to sport following anterior cruciate ligament reconstruction surgery: A systematic review and meta-analysis of the state of play.” British Journal of Sports Medicine. 2011;45:596–606.
4. McPherson A.L., Feller J.A., Hewettt T.E., and Webster K.E. “Psychological Readiness to Return to Sport is Associated with Second Anterior Cruciate Ligament Injuries,” American Journal of Sports Medicine. 2019;47:857–862.
5. Shah R.C., Ghagare J., Shyam A., and Sancheti P. “Prevalence of Kinesiophobia in Young Adults Post ACL Reconstruction.” International Journal of Physiotherapy and Research. 2017;5(1):1798–1801.
6. Hardy M.A. “The biology of scar formation.” Physical Therapy. 1989;69:1014–1024.
7. Gross M.J. “Chronic tendinitis: pathomechanics of injury, factors affecting the healing response, and the treatment.” Journal of Orthopaedic & Sports Physical Therapy. 1992;16:248–261.
8. Panariello R.A., Stump T.J.S., and Cordasco F. “The Lower Extremity Athlete: Post-Rehabilitation Performance and Injury Prevention Training.” Operative Techniques in Sports Medicine. 2017;25(3):231–240.
9. Panariello R.A., Stump T.J.S., and Allen A. “Rehabilitation and Return to Play following ACL Reconstructive Surgery.” Operative Techniques in Sports Medicine. 2017;25(3):181–193.
10. Panariello R.A., Stump T.J., and Maddalone D. “Post-Operative ACL Rehabilitation and Return to Play after ACL Reconstruction.” Operative Techniques in Sports Medicine. 2016;24(1):35–44.
11. Takarada Y., Takazawa H., Sato Y., Takebayashi S., Tanaka Y., and Ishii N. “Effect of resistance exercise combined with moderate vascular occlusion on muscle function in humans.” Journal of Applied Physiology. 2000;88(6):2097–2106.
12. Kacin A. and Strazar K. “Frequent low-load ischemic resistance exercise to failure enhances muscle oxygen delivery and endurance capacity.” Scandinavian Journal of Medicine & Science in Sports. 2011;21(6):231–241.
13. Jean L.M.Y., vonGaza G.L., Panariello R.A., and Chiu L.Z.F. “Unilateral Quadriceps Loading During Full Squat Exercise Without and With Single-Foot Elevation.” Unpublished manuscript.
14. Ebonie R., Purdam C., Girdwood M., and Cook J. “Isometric Exercise to Reduce Pain in Patella Tendinopathy In-Season; Is It Effective ‘on the road’?” Clinical Journal of Sports Medicine. 2019;29:188–192.
15. Wang R., Hoffman J.R., Tanigawa S., et al. “Isometric Mid-Thigh Pull Correlates With Strength, Sprint, and Agility Performance in Collegiate Rugby Union Players.” The Journal of Strength and Conditioning Research. 2016;30(11):3051–3056.
16. Townsend J.R., Bender D., Vantrease W.C., et al. “Isometric Midthigh Pull Performance Is Associated With Athletic Performance and Sprinting Kinetics in Division I Men and Women’s Basketball Players.” The Journal of Strength and Conditioning Research. 2019;33(10):2665–2673.
17. Lee M., and Carroll T.J. “Cross education: Possible mechanisms for the contralateral effects of unilateral resistance training.” Sports Medicine. 2007;37(1):1–14.
18. Farthing J.P., Krentz, J.R., Magnus, C.R. et al. “Changes in functional magnetic resonance imaging cortical activation with cross education to an immobilized limb.” Medicine and Science in Sports and Exercise. 2011;43(8):1394–1405.
19. Heady A.M., Spittle M., and Kidgell D.J. “Cross education and immobilization: Mechanisms and implications for injury rehabilitation.” Journal of Science and Medicine in Sport. 2012;15:94–101.
20. Magnus C.R., Arnold C.M., Johnston G., et al. “Cross-education for improving strength and mobility after distal radius fractures: a randomized controlled trial.” Archives of Physical Medicine and Rehabilitation. 2013;94(7):1247–1255.





