In a recent conversation with a group of physical therapists, athletic trainers, and strength and conditioning coaches, the subject matter progressed to an MVP NFL quarterback who had recently laterally dislocated his patella during a game day competition. When the discussion evolved to the rehabilitation and the post-rehabilitation “return to play” (RTP) training of this athlete’s knee, two suggestions mentioned for inclusion in the program design were the isolated strengthening of the vastus medialis obliquus (VMO) muscle and the stretching of the iliotibial band (ITB).
Neither isolated strengthening of the vastus medialis obliquus muscle nor stretching of the iliotibial band should be in the program design for the rehabilitation of an athlete’s knee. Share on XWhile the intention of these recommendations is commendable, I am concerned because these exercise philosophies were documented as fallacies decades ago. Although these viewpoints are without substance, there appear to be professionals who still accept and validate these myths.
The Vastus Medialis Obliquus
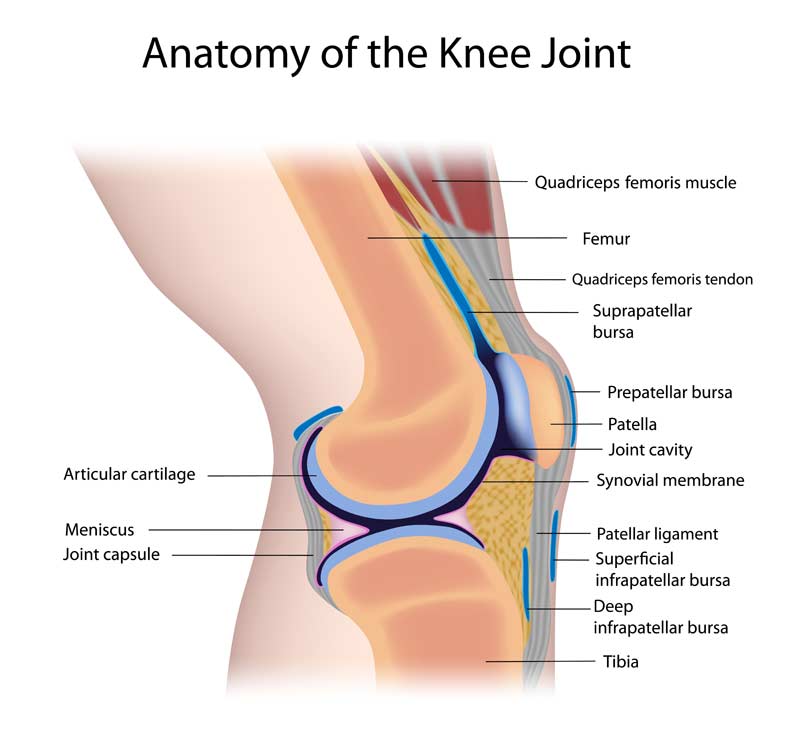
Patellofemoral pathology is a fairly common condition observed in the training room, clinical setting, and athletic performance enhancement environment. Pathologies may range from patellofemoral pain to the postoperative care of the repaired medial patella soft tissue stabilizers—i.e., vastus medialis/medialis obliquus (VMO), medial retinaculum, medial patellofemoral ligament, etc. (figure 1)—that may be disrupted after a lateral patella dislocation. Whether addressing an athlete’s patellofemoral pain or postoperative knee condition, physical rehabilitation and RTP training are essential to ensure an optimal RTP outcome.
Many rehabilitation and performance enhancement training program designs may include exercises that attempt to isolate the vastus medialis obliquus muscle to address the previously mentioned knee condition. Although this VMO exercise isolation “myth” was negated at least 20 years ago1,2, it continues to endure. The attempt to isolate VMO muscle activity may include, but is not limited to, the following exercises:
- Quad sets.
- Terminal open and closed kinetic chain knee extension exercises (TKEs) (figures 2a and 2b).
- Straight leg raises (SLR) with external rotation of the lower extremity (figure 3).
Athletes may or may not perform these exercises with the adjunct application of electric stimulation.
Many rehab and performance enhancement training programs include exercises that attempt to isolate the VMO even though the exercise isolation “myth” was negated 20 years ago. Share on X
Although these exercises will enhance the strength of the quadriceps muscles, helping to resolve the athlete’s knee pathology, this improvement is not due to isolation of the VMO. In addition, the reasoning for why some professionals formulate the performance of SLR with external rotation is based on the false premise that externally rotating the femur will result in further activation of the VMO (as seen in figure 3).

The knee is a hinge joint, and during the execution of an SLR, the force of gravity will act in a perpendicular manner between the knee and ground surface. The quadriceps mechanism will now be required to resist the resultant force attempting to flex the knee, as this is the only contractile soft tissue structure that is capable of resisting that force. The quadriceps mechanism, like any other dynamic anatomical structure, can only resist this external force via the neural activation of the muscle group. The external rotation of the femur gives rise to the placement of stress on the medial collateral ligament (MCL), a static stabilizer of the knee (figure 4).
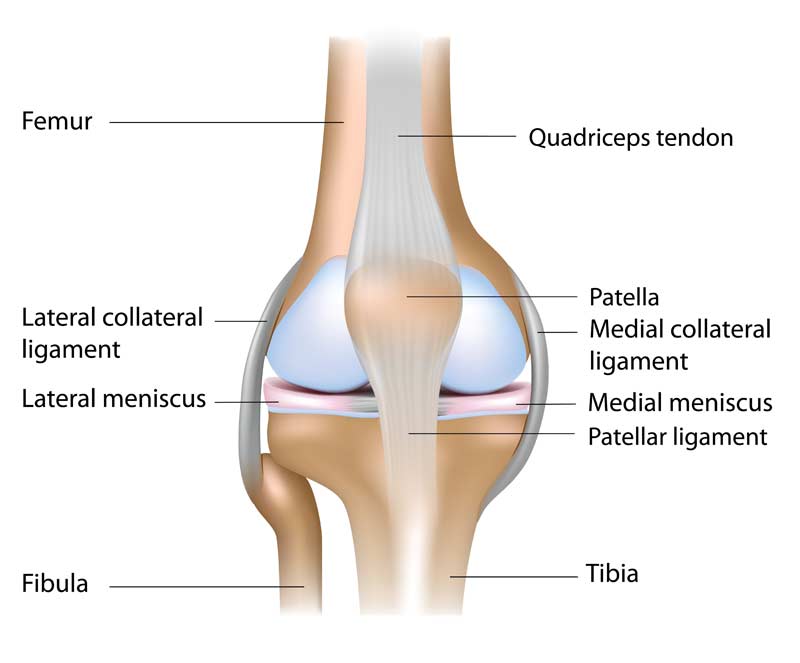
The external rotation treatment philosophy actually removes stress from the very muscle(s) practitioners are attempting to enhance. As an example, a patient with a diagnosis of polio, a condition affecting the anterior horn of the femoral nerve, or with a quadriceps tendon rupture can still perform a SLR when externally rotating their femur, based on the contributions of the adductor muscle group of the hip (adductor magnus, longus, and brevis, pectineus, gracilis, and obturator externus) via innervation from the obturator nerve, as well as the static stabilizing properties of the MCL. Therefore, we may ask why a professional who is attempting to activate and enhance the quadriceps muscle group would perform the SLR exercise in the external rotation position.
The Anatomy and Neuroanatomy of the Quadriceps Muscle Group
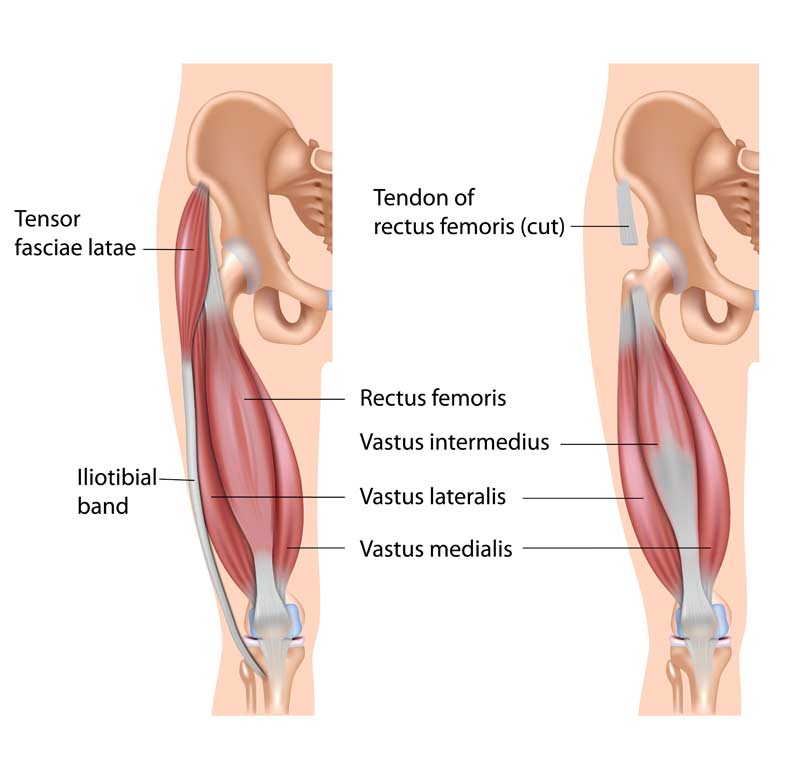
The quadriceps muscle group is comprised of the rectus femoris, vastus lateralis, vastus intermedius, and vastus medialis (figure 5).
The vastus medialis (VM) is located at the medial aspect of the muscle group. It consists of two separate components, the proximal vastus medialis longus (VML) and the distal vastus medialis obliquus (figure 6).4
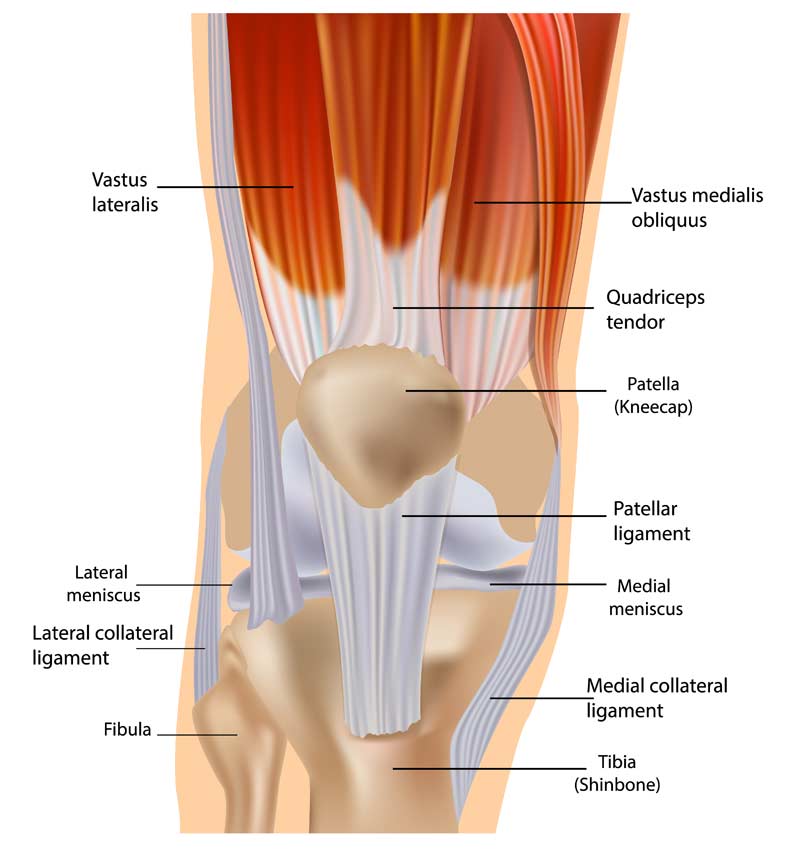
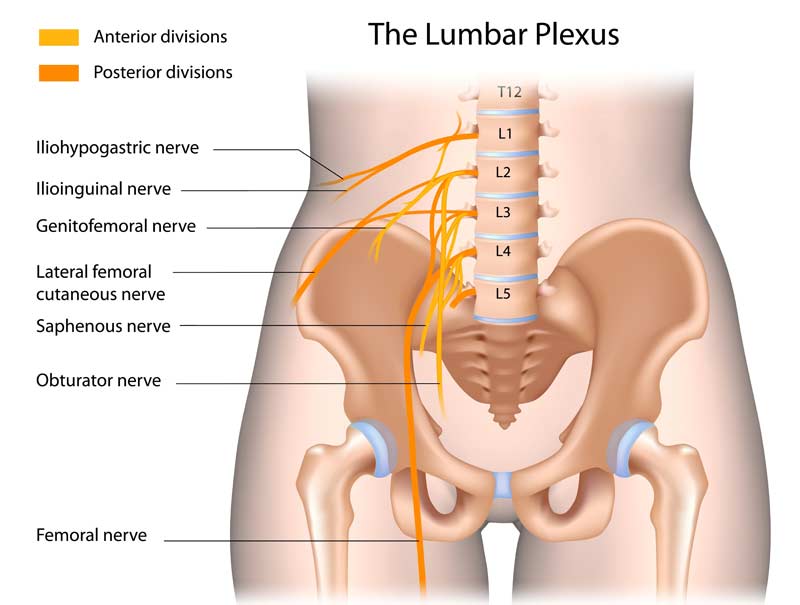
The neuroanatomy of the quadriceps muscle complex reveals an innervation from the femoral nerve (figure 7). The femoral nerve consists of large motor units that innervate all four heads of the quadriceps without individual fine motor unit innervation of the separate muscle heads. Therefore, since the vastus medialis does not have a distinct and separate nerve innervation (nor does the VMO), it is not possible to “isolate” this muscle from the other quadriceps muscles via a specific exercise performance.
To use a light switch as an analogy, if a single light switch (femoral nerve) is constructed to turn on all of the lights in four separate and distinct rooms (quadriceps muscles), how would it be possible to have this specific light switch turn on the lights in only one specific room?
The most beneficial way to enhance the VMO is to incorporate the same exercise philosophy used to improve any other muscle or muscle group, the application of unaccustomed stress. The application of unaccustomed yet safe levels of programmed stress is simply known as the “overload principle.” This principle may be accomplished most commonly in two ways: expose the athlete to higher levels of unaccustomed yet appropriate external resistance (i.e., weight intensity) or “overload” the athlete by increasing the velocity of the executed movement. Both of these methods will result in a positive adaption of the entire quadriceps muscle group.
Stress spreads throughout the kinetic chain of the lower extremity during the performance of activities of daily living (ADLs), as well as athletic endeavors. Thus, the activities prescribed for patellofemoral pathology should also include exercises that place emphasis upon the hip and the foot and ankle musculature. “Critical thinking” is a requirement for the approach to the athlete’s optimal exercise selection and program design. The rehabilitation and performance enhancement professional’s obligation to provide optimal treatment and/or performance enhancement training does not include the application of myths or fables during the programming of the exercises to be executed.
The Iliotibial Band
An additional suggested treatment and performance enhancement training strategy that came up during the aforementioned patella injury discussion is the “stretching” of the iliotibial band (ITB). This is another misconception that has also stood the test of time. The ITB is a distal continuation of the fascia arising from the tensor fascia lata (TFL), gluteus maximus, and gluteus medius muscles. The ITB serves as a supportive fascial structure that encapsulates the TFL muscle proximally and spans laterally along the lower extremity to attach to Gerdy’s (anterolateral tibial) tubercle (figure 8).

Many rehabilitation and performance enhancement professionals utilize various manual and commercial (foam rollers) soft tissue techniques in an attempt to “stretch” the ITB. However, the question arises, can the ITB really be stretched? The answer is no, it cannot. With specific regard to the ITB, a demonstrated predicted load of 2,040 pounds (927 Kg) and a force of 1,015 pounds (461 Kg) are needed to produce 1% of compression and shear forces, respectively5, upon this anatomical structure. It is highly doubtful that any manual technique or commercially applied soft tissue device can reproduce these high forces.
The ITB has also been utilized as an autograft of choice for primary anterior cruciate ligament reconstructions (ACLRs)6, physeal-sparing ACL procedures in skeletally immature prepubescent children7, ACLR lateral sling augmentation8, and the reconstruction of the anterolateral (ALL) ligament of the knee9. If this anatomical soft tissue structure “stretched out,” so to speak, how could the ITB possibly be considered as an appropriate surgical graft choice in restoring knee stability via ACL reconstruction surgery?
What Part of This Complex Does Stretch?
If a lengthening of the lateral soft tissue structures of the lower extremity is desired, there does appear to be a potential elongation of soft tissue at the proximal iliotibial band-tensor fascia lata complex (ITBTFLC), as well as at the gluteal region.10,11 The increased lengthening response in the proximal lower extremity region is likely due to the presence of the TFL, the area where greatest deformation with the least resistance to applied stress occurs, while elongation in the mid to distal aspect of the ITB does not result in length changes.10
Foam rolling directly over the ITB also results in no increase in hip adduction (soft tissue lengthening) range of motion (ROM), as measured by a modified OBER test.11 However, foam rolling over the soft tissue gluteal region, where the fan-shaped fibers converge and blend with the ITB superficially, resulted in an immediate and significant increase (soft tissue elongation) in hip adduction ROM.11 When applying techniques for desired soft tissue elongation to the lateral aspect of the lower extremity, areas of focus should include the gluteal region and the ITBTFLC, as placing emphasis directly upon the ITB will not result in a lengthening of this anatomical soft tissue structure.
Since you’re here…
…we have a small favor to ask. More people are reading SimpliFaster than ever, and each week we bring you compelling content from coaches, sport scientists, and physiotherapists who are devoted to building better athletes. Please take a moment to share the articles on social media, engage the authors with questions and comments below, and link to articles when appropriate if you have a blog or participate on forums of related topics. — SF
References
1. Cerny, K. “Vastus medialis oblique/vastus lateralis muscle activity ratios for selected exercises in persons with and without patellofemoral pain syndrome.” Physical Therapy. 1995; (8):672–83.
2. Malone, T., Davies, G., and Walsh, W.M. “Muscular control of the patella.” Clinical Sports Medicine. 2002; 21(3); 349–362.
3. Hubbard, J.K., Sampson H.W., and Elledge, J.R. “The Vastus Medialis Oblique Muscle and Its Relationship to Patellofemoral Joint Deterioration in Human Cadavers.” Journal of Orthopaedic & Sports Physical Therapy.1998; 28(6):384–391.
4. Weinstabl, R., Scharf, W., and Firbas, W. “The extensor apparatus of the knee joint and its peripheral vasti: anatomic investigation and clinical relevance.” Surgical and Radiologic Anatomy. 1989; 11(2):17–22.
5. Chaudhry, H., Schliep, R., Ji, Z., Bukiet, B., Maney, M., and Findley, T. “Three-dimensional model for deformation of human fasciae in manual therapy.” The Journal of the American Osteopathic Association. 2008; 108(8):379–390.
6. Stensbirk, F., Thorborg, K., Konradson, L., Jorgensen, U., and Holmich, P. “Iliotibial band autograft vs. bone-patella- tendon- bone autograft, a possible alternative for ACL reconstruction: A 15-year prospective randomized control trial.” Knee Surgery, Sports Traumatology, Arthroscopy. 2014; 22(9):2094–2101.
7. Kocher, M.S., Heyworth, B.E., Fabricant, P.D., Teplot, F.A., and Micheli, L. “Outcomes of Physeal-Sparing ACL Reconstruction with Iliotibial Band Autograft in Skeletally Immature Prepubescent Children.” Journal of Bone and Joint Surgery. 2018; 100(13):1087–1094.
8. O’Brien, S.J., Warren, R.F., Wickiewicz, T.L., Rawlins, B.A., Allen, A.A., Panariello, R.A., and Kelly, A.M. “The iliotibial band lateral sling procedure and its effect on the results of anterior cruciate ligament reconstruction.” American Journal of Sports Medicine. 1991; 19(1):21–25.
9. Stuyts, B., Van der Eeden, E., and Victor, J. “A New Reconstructive Technique of the Anterolateral Ligament with Iliotibal Band-Strip.” The Open Orthopaedics Journal. 2017; 11:321–326.
10. Wilhelm, M., Matthijs, O., Browne, K., Seeber, G., Matthijs, A., Sizer, P.S., Brismee, J., James, C.R., and Gilbret, K.K. “Deformation Response of the Iliotibial Band-Tensor Fascia Lata Complex to Clinical-Grade Longitudinal Tension Loading In-Vitro.” International Journal of Sports Physical Therapy. 2017; 12(1):16–24.
11. MacGregor, H. and Smith, J.C. “The Effects of an Acute Bout of Foam Rolling on Hip Range of Motion on Different Tissues.” International Journal of Sports Physical Therapy. 2018; 13(4):652–660.





