[mashshare]
Probiotic supplementation is a functional and practical nutritional strategy that powers an athlete’s health for optimal performance and protects an athlete’s future. The latest research suggests most health problems start in the gut. Therefore, gut microbiota is targeted as a potential therapeutic source for the treatment of certain diseases.
Diet has the greatest impact on gut microbiota composition. Yet, many athletes’ guts are currently a breeding ground for bad bacteria. Meal plans that enhance gut health look great on paper, but let’s be real—athletes are not following that meal plan daily and probiotic-rich foods may be neither effective nor practical to consume every day.
In this article, I’ll discuss why Olympians, recreational athletes, and those simply participating in physical activity need probiotics as an insurance policy for exercise, health, and longevity.
Poor Gut Health Is the Source of Many Athletes’ Health Problems
Imagine the pre-race anxiety (e.g., “butterflies in your stomach”) that hurts your push-off from the starting line or your mood that impacts your relationships with others during your hardest training week. Cue to your gut dictating your emotions. Your gut constantly communicates (via nerves and chemical signals) with your brain. Your brain listens to your gut microbiota.
Imagine training through a pounding headache, stuffy nose, sore throat, and fatigue that shows no sign of letting go during the two weeks leading to the peak of in-season. Imagine you haven’t been consistently showing up to your favorite group fitness class because of a recurring cold. Cue to the high training load, poor nutrition, and lack of sleep that increased your risk for infection and led to your limited ability or inability to train, and an ultimate decline in your performance.
Remember the worries about athletes’ exposure to filthy water supply and pollution during the Rio Summer Olympics? Does “super bacteria” ring a bell? Imagine all of the athletes’ hours of sacrifice and sweat during the last four years of training at the Olympic Training Center, only to get to the Games and have to compete for gold with gastrointestinal (GI) distress because of a weakened immunity that led to infection.
Everyone who exercises—from Olympians to recreational athletes to those simply doing physical activity for well-being and enjoyment—can relate to the frustration of these common situations, which originate from the state of a person’s gut health.
The gut is at the intersection of our risk for disease. Share on XFurthermore, causes of mortality (e.g., obesity, diabetes, cardiovascular disease, cancer) and chronic conditions (e.g., inflammatory bowel disease, asthma, allergies, rheumatoid arthritis) are all linked to gut microbiota dysbiosis (the imbalance of good and bad bacteria). The gut is closely linked to the proper functioning of our metabolism, immunity, and brain. Therefore, the gut is at the intersection of our risk for disease.
What Is a Healthy Human Microbiome?
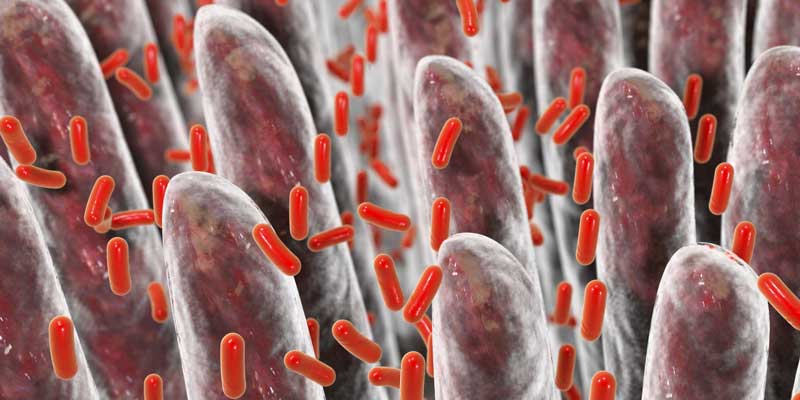
The human body has communities of microbiota living on the surface and inside. These communities of microbiota are instrumental to our physiology, immunity, digestion and absorption, detoxification processes, brain health, and risk for disease. For example, some gut microbiota can create proteins that we need for our health (e.g., enzymes to break down certain foods, vitamin synthesis, etc.)
We have two genomes: we inherit one from our parents and the other is a microbiome that we acquire (i.e., the genome of each of our resident microbiota). The difference between the two genomes is:
- Inherited genome: stable throughout our life
- Microbiome: changes constantly and impacted by many factors, such as diet, age, travel, therapies, hormonal cycles, and illness.
The development of our gut microbiota composition starts at birth (e.g., delivery method) and continues to evolve throughout our life. The fluctuation in our microbiome (good and bad) happens easily and results from environmental factors and stressors that we face daily, especially people who exercise.
Gut research is in its infancy, but we know that the:
- Gut microbiota composition and microbiome impact our health because of their role in our physiology and development of organs;
- Gut is a complex ecological system impacted by host and environmental factors; and
- Regulation of gut microbiota to reach a healthy status is a challenge.
A healthy human microbiome needs gut microbiota that are diverse, balanced, and stable.1 The problems arise when our gut experiences microbial dysbiosis (i.e., a disruption in the balance of microbiota). This results from fewer bacterial species that enhance health; less diversity of bacterial species; and higher disease-causing bacteria.2
These factors that cause dysbiosis are influenced by:
- General lifestyle (e.g., diet)
- Genetics
- Birth
- Health/disease
- Medication
Daily stressors (e.g., dietary factors, training load, pollution, travel, poor sleep, etc.) experienced by everyone, especially athletes, increase the risk for dysbiosis.
Of all the factors impacting the gut microbiome, diet may have the largest effect, and it is one of the only stressors within our control. Dietary changes can quickly change our gut microbiota composition; in fact, they cause up to 57% of gut microbiota changes.3 Therefore, a good strategy is to follow a balanced diet and healthy lifestyle.
But that’s not always practical. How many people (especially athletes) know what dietary factors can help gut health, let alone follow through with it daily? (I discuss this more below.)
Also, athletes and fitness enthusiasts are not models for a healthy lifestyle—so these populations can really benefit from supplementing with probiotics—“live microorganisms which, when provided in adequate amounts have a health benefit on the host” because of their impact on the gut and their help in preventing or improving many different health conditions.
Additional factors to reverse or prevent dysbiosis include sound nutrition, specific probiotics, and prebiotics.
Dietary Factors That Affect Gut Health
It’s out of the scope of this article to describe every dietary factor that impacts our gut, so this is just a summary.
What you habitually consume will impact your gut the most. Share on XThe impact of diet breaks down into:
- Dietary patterns (e.g., Western Diet, vegetarian diet);
- Food components (e.g., fiber, carbohydrate, fat, protein, phytochemicals);
- Specific foods (e.g., whole grains, fruits, nuts, vegetables, legumes); and
- Food-associated microbes.
Of all the factors that can impact the gut microbiome, a long-term diet might contribute the greatest effect. This means what you habitually consume will impact your gut the most.
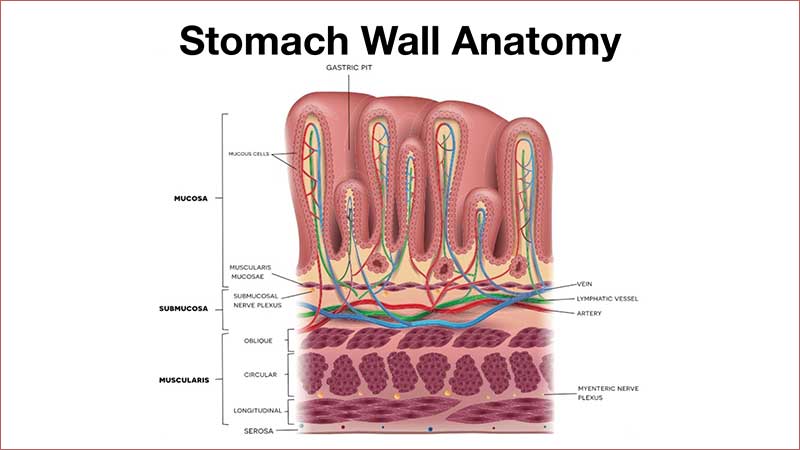
Western Diet
Geography, which corresponds with a particular diet in that location, can determine gut microbiota composition. The definition of a Western Diet (WD) is one that contains a high amount of fat (35-60% of total kilocalories) and added sugars, and is low in fiber. Some articles suggest that the WD fosters a pro-inflammatory gut environment.4,5 All of this is consequential to the gut microbiota because it weakens the gut barrier, which leads to toxins entering the bloodstream and inflammation to ensue. This is the reason the WD is linked to cardiovascular disease and diabetes, which are both associated with high inflammation in the body.
The WD displaces the wholesome foods we should be consuming, which hurts the diversity of our gut microbiota.
A recent study found that diet is a critical factor in causing microbial dysbiosis. In it, a WD had a greater impact on gut microbiota diversity than BMI in 81 Alabama residents age 33 (+/- 13.3) years with a BMI of 28.3 (+/- 7.01).
Essentially, the WD is a major factor in dysbiosis—more than being overweight or obese.
Because gut health is tied to brain health, the WD is also known to hurt cognition. How a WD impacts the brain is not really clear, but it may be due to the gut-brain-axis. A WD can shift microbiota composition, which may result in cognitive problems.
Routes that connect the WD with gut microbiota dysbiosis and cognitive decline, include:
- Gut barrier strength
- Blood brain barrier strength
- Neuroinflammation
- Weakened insulin signaling
All of these factors work together to influence brain function. The WD hurts gut barrier strength, which then allows bad substances to get into our body and potentially cause metabolic complications and cognitive dysfunction. This is a possible reason to link the WD with neurocognitive dysfunction.
Cue to the aging athlete’s future brain health.
Food Components and Specific Foods
The diversity and types of food dictate which microbes will colonize, grow, live, and get eliminated.6
Food components, such as dietary fiber (i.e., carbohydrate that is neither digested nor absorbed by humans), can provide food for gut microbiota. But different bacteria specialize in the fermentation of different fibers. Therefore, complex diets can either be growth-promoting or growth-inhibiting.
The by-products of bacterial metabolism, such as vitamins and short-chain fatty acids (SCFAs), are critical for our health because they have health-promoting effects. A WD hurts the production of SCFAs,7 so systematic inflammation in the gut increases and neuroprotection of the brain decreases.

Low dietary fiber intake corresponds with lower microbiota diversity, more anti-pathogenic bacteria, and lower SCFA production.8 Low fiber and resistant starch intake may result in a loss of gut microbiota diversity and function.9 Diets high in simple and refined carbohydrates do not promote healthy gut microbiota nor do they allow gut microbes to generate the SCFAs.10
Whole grains typically contain lots of dietary fiber, but the average dietary fiber intake in the U.S. is 15 g/day (60% of what women need and 40% of what men need). Red berries, including red wine, that contain anthocyanins have increased Bifidobacterium in many studies.11,12</sup Pistachios have produced a greater impact on microbiota composition compared to almonds.
But are athletes routinely consuming these foods, especially in the context of the prevalent Western Diet?
Evidence-Based Research on Probiotic Supplementation Helping Alleviate Daily Stressors
Probiotic supplementation has shown to be effective and necessary for enhancing health in trained individuals, especially related to lowering the risk for respiratory and gastrointestinal (GI) complications during high-stress periods in training and competition.
Typically, studies determine the effects of probiotics by examining clinical measures of immune function and illness. The most commonly studied species in athletes and active people include:
- Lactobacillus casei
- L. fermentum
- L. acidophilus
- L. rhamnosus13
Here’s a summary of a few studies investigating the influence of probiotic supplementation on the typical stressor burdens on athletes and non-athletes.
GI Complication Severity
Lowering gut permeability helps with strengthening our immunity. Multi-strain probiotics consumed daily have shown to improve gut barrier strength in endurance athletes. Clinical trials using a multi-strain probiotic (L. acidophilus, B. lactis, and B. bifidum) helped significantly improve irritable bowel syndrome complications and stopped the increase in the antibiotic resistant strain, enterococci.

For those who think probiotics are only for athletes, a study using recreational athletes training for their first long-distance triathlon found that taking a multi-strain probiotic combined with prebiotics and antioxidants at 30 billion colony forming units (CFU, the unit of measurement for probiotics) per day for 12 weeks before their triathlon may have provided support in reducing GI symptoms because of the increase in gut barrier strength. The inclusion of antioxidants may have been an additive benefit because they lowered endotoxin (toxins from bad bacteria) levels.
Ultimately, this strategy showed promise in those athletes beginning endurance training, especially those who are prone to GI complications.
To learn more about how probiotic supplementation helps alleviate GI complications and are beneficial for the treatment and prevention for GI diseases, read this meta-analysis.
Upper Respiratory Tract Infections Associated with Training
Upper respiratory tract infections (URTIs) are around 35-65% of the illnesses seen in sports medicine. However, athletes do not have more URTIs than non-athletes—both have the same incidence.14
Athletes with this persistent illness obviously experience a negative impact on health and performance (as evidenced in swimmers), especially during times of strenuous training. Distance runners experience URTIs more frequently following competition.15 This is when probiotic supplementation becomes a powerful nutritional strategy to lower an athlete’s susceptibility to illness.
The most consistent biomarker to identify and monitor athletes at risk for URTI is measuring salivary immunoglobulin A (IgA), which offers protection against infections at mucosal surfaces and maintenance of the gut barrier.

Using salivary IgA as a biomarker is not practical because of the lab testing required. Until then, we don’t necessarily have a systematic way of monitoring an athlete’s immune status. Yet, studies in elite athletes from different sports have found that an increased risk for URTIs corresponds with low levels of salivary IgA,16,17 low pre-season salivary IgA levels,18 and declining levels over a training period.19
As for non-athletes, salivary IgA decreases during and after high-intensity exercise.20
To lower the risk for and impact of URTIs, nutritional interventions need to focus on improving immunity and/or lowering inflammation.
Athletes have undergone supplementation with different strains of Lactobacillus. A study showed that eight weeks of supplementation with L. casei reduced the number of URTIs, including symptom severity and duration. Another study showed L. fermentum supplementation for one month also decreased the number of days of URTI and severity of symptoms in distance runners.
Maintaining immune health to prevent URTIs would require changing training regimes, better managing daily stressors, and regularly consuming a probiotic-rich diet. However, this is not necessarily practical. Hence, probiotic supplementation is warranted. Read more on how probiotics can strengthen our immunity.
Inflammation
Athletes experience chronically low levels of inflammation. But over time, this inflammation can grow and lead to poor health, less physical activity, and a propensity to diseases related to chronic inflammation, such as cardiovascular disease and mental disorders.
Serum C-reactive protein (CRP) is a biomarker for systemic inflammation—with high levels found in many chronic conditions, such as cardiovascular disease, obesity, type II diabetes, high blood pressure, high fasting blood glucose, and low HDL.
A recent meta-analysis concluded that probiotic supplementation may lower CRP levels. The mechanisms may be due to probiotic effect on inflammation by preventing or repairing “leaky” gut linings and stopping pro-inflammatory responses.21 Probiotics also increase SCFAs that provide anti-inflammatory functions.
Of course, more clinical trials are needed, especially to determine the exact dose and strains of probiotic supplements needed for each disease. But for now, the potential protective effect that gut microbiota has in managing our inflammation balance is critical to the prevention of disease.
International Travel
There is an increased risk of GI problems during international travel. Typically, good hygiene helps to prevent bacterial contamination and spread, but much of the time that is not enough. Therefore, probiotic supplementation for athletes traveling abroad is a critical part of a sports immunonutrition prevention plan.

Recommendations Regarding Probiotic Supplementation
When the gut becomes weak, bad substances can enter the blood, ignite inflammation, lower immunity, hurt performance and overall health, and reduce longevity.
It has been suggested that studies investigating probiotic supplementation in athletes “provide modest evidence that probiotics can provide some clinical benefits in athletes and other highly active individuals.” Also, probiotic supplementation in combination with other dietary strategies could help athletes with a history of gut complications. The benefits in managing URTIs may be useful for those who continually experience symptoms of the common cold or flu.
A 2016 review, “Immunological aspects of sports nutrition,” suggests that daily consumption of probiotics is currently one of the dietary strategies offering the best chance of success at maintaining a strong immunity.
The latest systematic review regarding effectiveness of probiotics in healthy children and adults concluded that, in those supplementing with a probiotic, there were significantly fewer days of illness, shorter durations of illness, and fewer number of days absent from work.
A review on endurance exercise and gut microbiota states that probiotics is the main dietary strategy to modulate gut microbiota. Furthermore, providing different Lactobacillus and Bifidobacterium strains to athletes may help maintain overall health, enhance immunity, improve gut barrier strength, and lower oxidative stress.
Athletes and coaches need to consider the extent to which there is a translational outcome or an important clinical benefit.
Of course, more research will help us better understand the bacterial strains, their mechanisms, and best practices for probiotic supplementation, especially in relation to the specific health benefit desired (e.g., lowering URTIs, preventing GI complications, etc.). But right now, incorporating a probiotic supplement with current evidence-backed strains and at an efficacious dose is the best guideline we have for using a nutritional strategy to potentially correct certain immune and GI problems, and potentially lower risk for certain diseases.
Bottom Line: Everyone can benefit from the right probiotic supplement to enhance gut health.
Should We Supplement with Probiotics?
Let’s discuss whether we should incorporate a probiotic supplement by using the Guru Performance Institute’s food-first approach in its Position Stand on Practical Considerations for Supplement Use in Sport.

Balanced Diet. A balanced diet should be the foundation of an athlete’s diet, but that’s not always the case. It’s difficult to achieve a balanced diet given the prevalence of the WD, and athletes’ diets are typically nutrient-poor and energy-dense. In some athletes, diets are nutrient-poor combined with energy-poor.

Sports Nutrition. Nutrition for sport performance or exercise needs to focus on more than just immediate performance. There are many touted “food is fuel” nutritional strategies. At the basic level, fueling for acute performance—which is typically the athlete’s main dietary pattern, as nutrition periodization tailored to training periodization is only gradually gaining traction—can potentially damage the gut.
Then, there’s fueling at the professional/elite/Olympic level. While we don’t know everything that happens behind closed doors, we’ve seen the prescribed meal plans of many professional athletes on paper. These meal plans are the “what” and “how.”
An athlete may not always follow that written prescribed diet from the sports nutritionist, and diet can change the gut environment within just a few days. The gut microbiota composition is shaky if an athlete only follows the prescribed meal plan a few days per week.
On top of that, how many of these meal plans (or buffet line management) are strategically designed to optimize the athlete’s gut health? In other words, look at the meal plans or buffet options and identify which dietary pattern is most obvious and which food components and probiotic-rich foods they include.
For sports nutritionists against probiotic supplementation, are you adding probiotic-rich foods/beverages to the athlete’s meal plan or incorporating them at the training tables or buffet options? The message and practice don’t always align.

I’ll admit, it’s a challenge to design a meal plan or diet that increases the number of microbiota, and have it followed daily. Even if the meal plan is part of a gut-enhancing diet, there are still a few barriers to gut health optimization.
- Consumer (athlete) choice is a major factor:
- Athletes don’t have to eat what they’re given or told to eat (e.g., “big boy” rules).
- Athletes don’t have to follow nutritional guidelines.
- In reality, these meal plans:
- Do not necessarily reflect the athlete’s “why”—why should they follow this nutritional guidance.
- May just look great on paper. We don’t know if words on paper translate to behavior, especially sustained behavior, which goes back to the “why.”
This is where the attitude of the athlete toward performance, overall health, and longevity dictates the effectiveness of nutrition. This is where we need to tackle their “why” and make sure it’s a shared fundamental belief with gut health.

Identification of the Need to Supplement. When implemented correctly, a supplement can help improve health, recovery, and performance.
Is there a genuine need to supplement? For gut health, the answer is “yes.” After a holistic review of the athlete’s diet, probiotic supplementation is usually warranted.
Probiotics are typically consumed from fermented milk products (e.g., yogurt), kefir, sauerkraut, etc. The main probiotic bacteria in dairy products include L. acidophilus, L. casei, and Bifidobacteria.
Eating probiotic-rich foods alone doesn’t hold a candle to supplementing with the right probiotic. In fact, probiotics from food are a perfect example of how a “balanced” diet may not work if you want to take full advantage of probiotics.
Practically speaking, some foods can be consumed every day (e.g., eggs, nuts, energy bars, etc.), but probiotic-rich foods (e.g., yogurt, kefir, sauerkraut, etc.)—likely, not so much. And that’s okay. After all, you’d have to have 2-25 servings of yogurts per day to maintain good gut health, and that’s probably not practical.
Consuming a small dose of probiotics—which may not be a realistic daily habit—doesn’t even make a dent in your daily overall need AND the needs for the rest of your life. The dose of probiotics needed is not easily obtainable through diet. The therapeutic benefits of probiotics are strain-specific and the dose is critical for efficacy.
A recent study investigating the Canadian food supply found that the probiotic dosages in most food products are too low to provide the health benefits found in clinical trials. For example, Danone’s DanActive has the strain Lactobacillus casei DN 114-001—shown to decrease the risk and duration of certain conditions, such as URTIs, sore throats, and influenza in adults, children, and the elderly. However, the probiotic dosage used in the studies was three times higher than that in one serving of DanActive.
It was also reported that nine brands provided the species name but did not identify the strain, so it was difficult to tell their product’s specific probiotic health benefits. Most of the products had one or two strains.

Kefir (a fermented milk with probiotics added) products provided the most strain and species diversity and the highest dosage (45 billion CFUs per serving). Yet, there was still variability in dose and diversity among the kefir products.
Key points from the study:
- To get the health benefits found in the studies, you would need to eat between two and 25 servings of “probiotic” products per day.
- Most products provide one billion CFUs of probiotics because this is the minimum amount required in Canada to provide “core” benefits. This allows for a company to claim their product “promotes a healthy gut flora.”
- Most products provided one or two strains. Yet, the science shows that multi-strain formulas may be more effective than single strains because different probiotics can work synergistically with their health effects.22 For example, L. acidophilus combined with Bifidobacterium lactis has shown to lower the risk of fever, coughing, and rhinorrhea.
- Currently, there’s no consensus on what strain, dose, or product is the best.
Therefore, only following a food-first approach with probiotics will most likely lead to a suboptimal intake.
Given that many athletes do not adhere to a balanced diet or individualized sports nutritional advice, supplementation is warranted. Yet, is a probiotic supplement really a supplement? Probiotics can be considered a “food,” as they are a nutritious substance that we eat or drink to maintain life and growth. Probiotics can also be considered a “functional food” because they constitute a food with an additional function—to promote health and prevent disease. So, what’s the difference if probiotics are in a yogurt, a drink, or a pill?
Just following a food-first approach with probiotics will most likely lead to a suboptimal intake. Share on XGranted, a single supplement isn’t a cure-all, but given that few probiotic-rich foods get consumed daily, probiotic supplementation is a safe health insurance policy.
Sound Probiotics: Engineered for the Competitive Athlete, but Beneficial for Everyone
The investment in making the athlete’s best interest our best interest led to us using sports nutrition to not just optimize performance, but to protect the athlete’s health in the future.
Unavoidable hard training and daily stressors, and a typically nutrient-poor, energy-dense dietary pattern predisposes athletes to a poor gut microbiota profile and many GI complications that lead to inflammation and potential long-term health consequences. How do we translate what we know about probiotics into a solution for athletes?

We focus on immunonutrition support to build a strong core of gut microbiota that strengthens the athlete’s gut wall lining and serves as a shield to protect against both the stressors the athletes face daily and aging. To accomplish this, the athlete’s diet needs to include probiotics. Sound Probiotics’ supplement is our nutritional weapon to optimize athletes’ power. It features eight probiotic strains, has 25 billion CFUs per capsule, and includes the prebiotic beta-glucan for synergistic effect.
There is no harm in choosing the right probiotic supplement even if mechanisms of various probiotic health benefits are not currently fully understood. Practically speaking, it makes sense to supplement with probiotics—whether it helps or simply has a neutral effect.
For athletes who need a “why”: Consider the value (investment) in adding a cost-effective, research-supported supplement created for you: to support your training demands, performance, overall health, and longevity.
Practical Advice
- Probiotic supplementation should begin at least two weeks before international travel, a major training cycle, or a competition so that there’s enough time for the bacterial species to colonize in the gut.
- Athletes and coaches should monitor tolerance and any side effects. Stomach rumbling and increased gas are typical experiences during the first few days because of the increased activity occurring in the gut.
- Athletes should take the probiotic supplement with food at the same time each day (e.g., breakfast).
- To measure gut health, start by looking at your diet, training load, prevalence of illness, mood, and fatigue.
Winning at Sport and Life Takes Guts
Gut microbiota is one of the fastest moving areas of research. Maybe one day we’ll even see personalized probiotics. The data is still being collected on all parts of health and respective mechanisms to determine how probiotics work, but there is enough data to support saying: Take a probiotic daily to get the extra edge in performance and health.
Of course, everyone should follow a gut-health friendly diet and eat probiotic-rich foods. But if you want to help athletes, use functional nutrition now by adding a probiotic supplement like Sound Probiotics to enhance health and performance so that athletes need less traditional medicine in the future.
The potential is so high you should start the habit today. In the end, you’ll win at both athletic and human performance.
Since you’re here…
…we have a small favor to ask. More people are reading SimpliFaster than ever, and each week we bring you compelling content from coaches, sport scientists, and physiotherapists who are devoted to building better athletes. Please take a moment to share the articles on social media, engage the authors with questions and comments below, and link to articles when appropriate if you have a blog or participate on forums of related topics. — SF
[mashshare]
References
- Lozupone CA, Stombaugh JI, Gordon JI, Jansson JK, Knight R. Diversity, stability and resilience of the human gut microbiota. Nature. 2012;489(7415):220-230.
- Petersen C, Round JL. Defining dysbiosis and its influence on host immunity and disease. Cell Microbiol. 2014;16(7):1024-1033.
- Zhang C, Zhang M, Wang S, et al. Interactions between gut microbiota, host genetics and diet relevant to development of metabolic syndromes in mice. ISME J. 2010;4:232–41.
- Greer JB, O’Keefe, SJ. Microbial induction of immunity, inflammation, and cancer. Front. Physiol. 2011;1:168.
- Wu SV, Hui H. Treat your bug right. Front. Physiol. 2011;2:9.
- Shanahan F, van Sinderen D, O’Toole PW, Stanton C. Feeding the microbiota: transducer of nutrient signals for the host. Gut. 2017;June29 pii:313872.
- Berger K, Falck P, Linninge C, Nilsson U, Axling U, Grey C, et al. Cereal byproducts have prebiotic potential in mice fed a high-fat diet. J. Agric. Food Chem. 2014;62:8169–8178.
- Konig D, Berg A, Weinstock C, et al. Essential fatty acids, immune function, and exercise. Exerc Immunol Rev. 1997;3:1–31.
- David LA, Maurice CF, Carmody RN, et al. Diet rapidly and reproducibly alters the human gut microbiome. Nature. 2014;505:559–63.
- De Filippo C, Cavalieri D, Di Paola M, et al. Impact of diet in shaping gut microbiota revealed by a comparative study in children from europe and rural africa. Proc Natl Acad Sci U S A. 2010;107:14691–6.
- Vendrame S, Guglielmetti S, Riso P, Arioli S, Klimis-Zacas D, Porrini M. Six-week consumption of a wild blueberry powder drink increases bifidobacteria in the human gut. J Agric Food Chem. 2011;59:12815-20.
- Zumaquero JM, Clemente-Postigo M, Estruch R, et al. Influence of red wine polyphenols and ethanol on the gut microbiota ecology and biochemical biomarkers. Am J Clin Nutr. 2012;95:1323-34.
- Pyne DB, West NP, Cox AJ, Cripps AW. Probiotics supplementation for athletes – clinical and physiological effects. Eur J Sport Sci. 2015;15(1):63-72.
- Fricker PA, Gleeson M, Flanagan A, Pyne DB, McDonald WA, Clancy RL. A clinical snapshot: do elite swimmers experience more upper respiratory illness than nonathletes? Clin Exerc Physiol. 2000; 2: 155–158.
- Nieman DC, Hanson DA, Dumke CL, Lind RH, Schooter LR, Gross SJ. Relationships between salivary IgA secretion and upper respiratory tract infection following a 160-km race. J Sports Med Phys Fitness. 2006; 46: 158–162.
- Gleeson M, McDonald WA, Cripps AW, Pyne DB, Clancy RL, Fricker PA et al. The effect on immunity of long-term intensive training in elite swimmers. Clin Exp Immunol. 1995;102:210–216.
- Nieman DC, Hanson DA, Dumke CL, Lind RH, Schooter LR, Gross SJ. Relationships between salivary IgA secretion and upper respiratory tract infection following a 160-km race. J Sports Med Phys Fitness. 2006;46:158–162.
- Putlur P, Foster C, Miskowski JA, Kane MK, Burton SE, Scheett TP et al. Alteration of immune function in women collegiate soccer players and college students. J Sports Sci Med. 2004;3:234–244.
- Gleeson M, McDonald WA, Cripps AW, Pyne DB, Clancy RL, Fricker PA et al. The effect on immunity of long-term intensive training in elite swimmers. Clin Exp Immunol. 1995;102:210–216.
- Gleeson M, Pyne DB. Exercise effects on mucosal immunity. Immunol Cell Biol. 2000;78:536–544.
- Mazidi M, Rezaie P, Kengne AP, Mobarhan MG, Ferns GA. Gut microbiome and metabolic syndrome. Diabetes Meta Syndr. 2016;10:S150–S157.
- Sanders ME. Summary of conclusions from a consensus panel of experts on health attributes of lactic cultures: Significance to fluid milk products containing cultures. J Dairy Sci 1993;76:1819–1828.




