Groin pain is a common occurrence in multidirectional field sport athletes. According to a 15-year prospective UEFA injury study, groin pain accounts for approximately 12%-16% of all time-loss injuries in men’s football (soccer).1 The complex anatomical nature of the region makes groin pain challenging to diagnose, manage, and rehab, with high recurrence rates of ~20% for many football athletes.2,4,5 The interactions and interconnections of muscles, ligaments, and tendons around the hip and pubic symphysis make it difficult to differentiate which structure is pain sensitive and which is the primary cause for pain.2,3
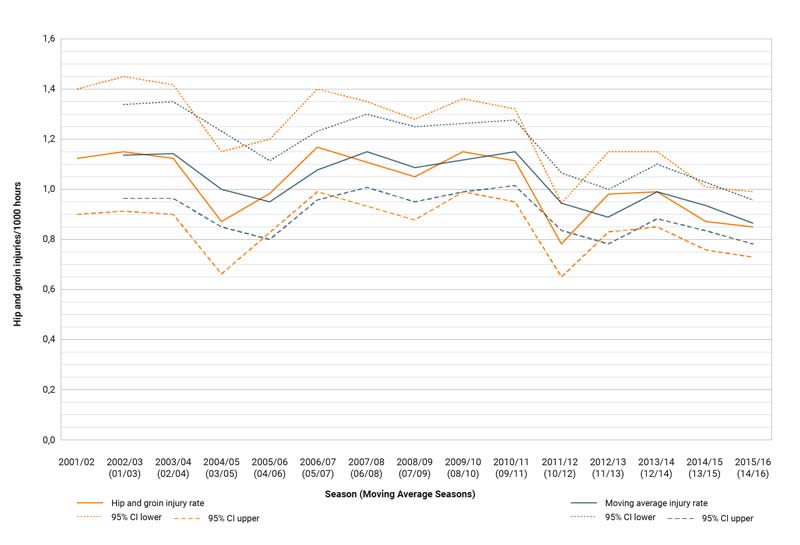
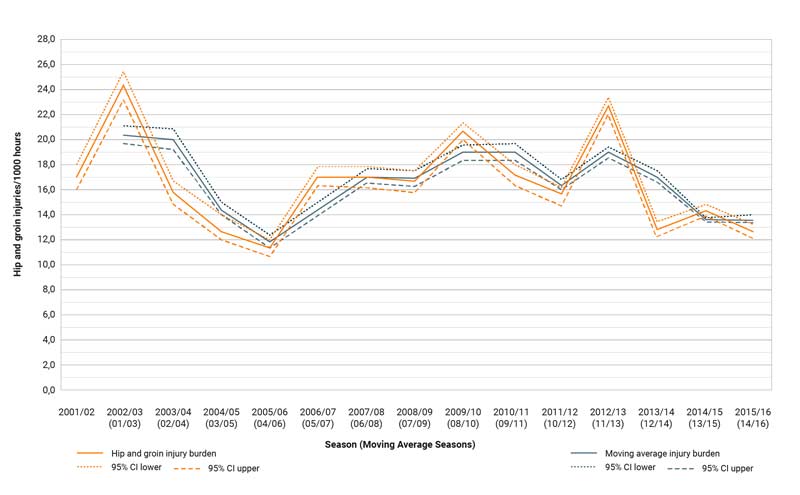
This trend in injury rates and severity highlights the complex nature of the region and the historical inconsistencies that have existed when it comes to diagnosing and defining groin pain. Share on XWhile the UEFA study does show the rate of hip and groin injuries have decreased slightly, (figure 1), the injury burden (figure 2) remains unchanged, even suggesting a slight increase in injury severity. This trend in injury rates and severity not only re-emphasizes the complex nature of the region, it also highlights the historical inconsistencies that have existed when it comes to diagnosing and defining groin pain.
Groin Pain Terminology and Diagnosis
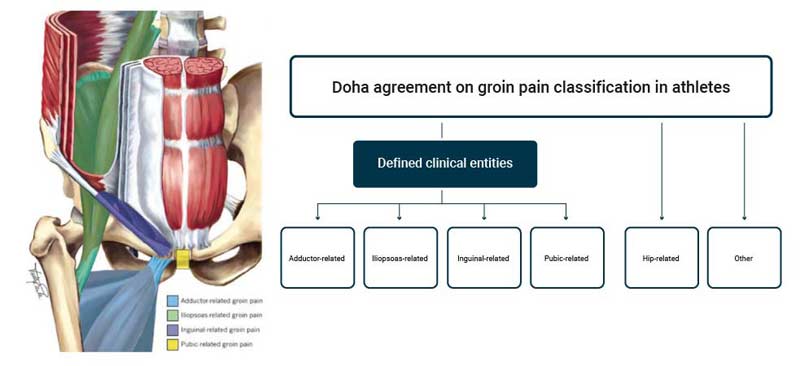
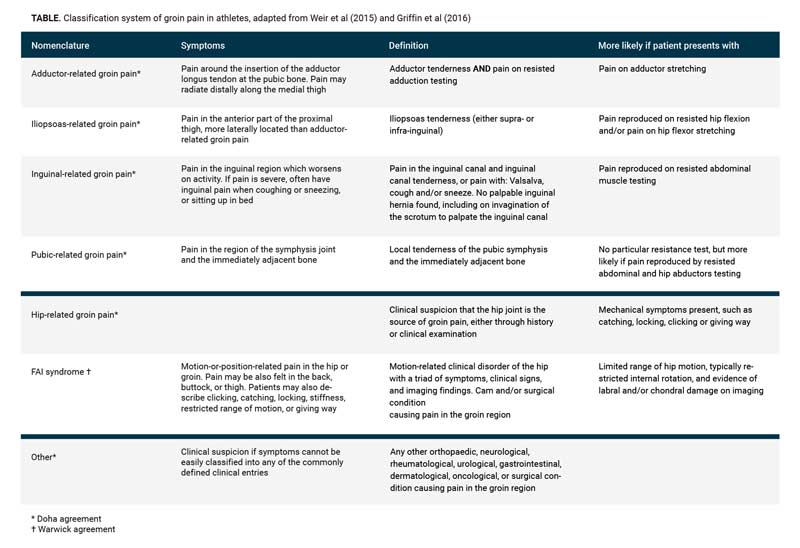
Until recently, there had been poor agreement on the diagnosis and terminology of groin pain. The Doha agreement2offers a global, standardized framework for groin pain and has been a positive development for consistency of diagnosis and terminology. The clinical entities as defined in the Doha agreement (see figure 3) can be used by practitioners to assist with clinical examination, exercise prescription, and return to performance guidelines. Another resource on groin pain diagnosis is this video from FIFA, which can help practitioners understand clinical differences during physical examination or when diagnosing different clinical entities of groin pain.
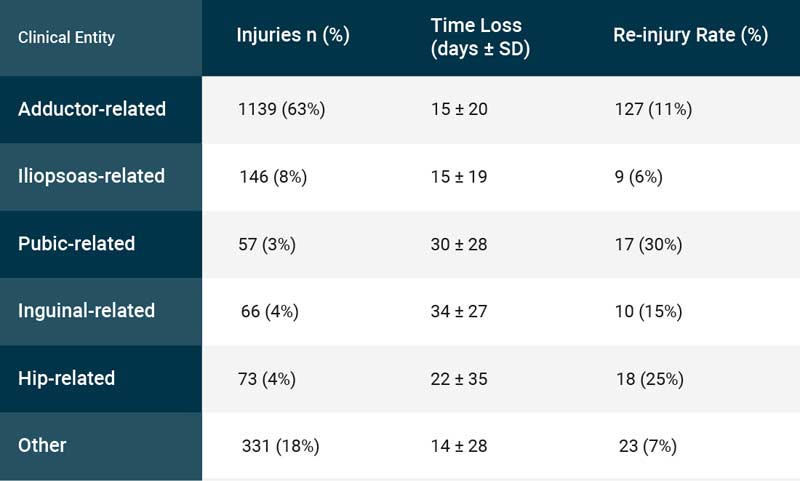
The most common type of groin injury is acute adductor-related pain (figure 4), which is likely to occur during activities such as change of direction or kicking. Despite acute pain being more common, it is gradual-onset or longstanding pain that is a greater cause for concern. Recent evidence suggests insidious onset pain may be responsible for a high number of undiagnosed or unrecorded groin injuries, which has resulted in athletes playing through pain or discomfort. These types of groin injuries are complicated, with the athlete often presenting with pain across multiple anatomical sites, acute pain at the tendon insertion, and possible boney edema on imaging (see figure 5).
If an athlete presents with such symptoms, or any clinical findings as defined within the Doha agreement, evidence recommends a comprehensive examination of the entire hip and groin region. It is worth noting that no current evidence suggests imaging can further assist with diagnosis or return to performance timeframes. This is important to consider when assessing an athlete with long-standing groin pain, as imaging is a common procedure but can often lead to overinterpretation of results. Rather, evidence supports groin pain diagnosis and prognosis be guided by the individual athlete’s symptoms, clinical presentation, and functional restrictions.
While imaging is a common procedure…evidence supports groin pain diagnosis and prognosis be guided by the individual athlete’s symptoms, clinical presentation, and functional restrictions. Share on XRisk Factors of Groin Pain
While injuries are multifactorial and unpredictable, a good level of evidence suggests the factors shown below may lead to an increased risk of groin injury.
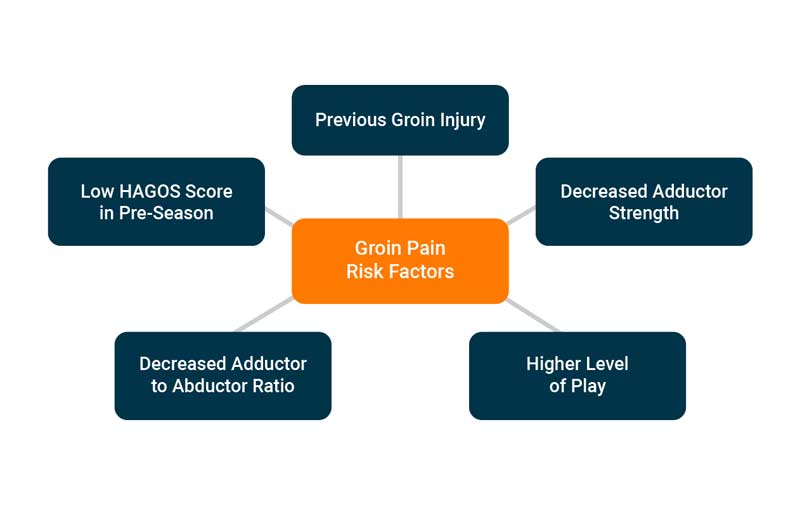
Other factors often associated within the literature include:
- Pain on hip adduction squeeze test.
- Reduced hip internal rotation.
- Reduced bent knee fallout range of motion.
It should be noted that there has been some conflicting evidence when discussing range of motion impairment and its association with groin pain.
Monitoring and Managing Groin Pain
As mentioned previously, the major concerns for hip and groin injuries are either insidious onset pain at multiple anatomical sites or long-standing groin pain that results in performance decrements. The key to successfully managing groin pain is to develop a monitoring framework that attempts to mitigate the risk of athletes developing insidious groin pain. Wolin et al. developed a framework of a monitoring system, useful for the early detection and management of groin pain8 (see the original framework here).
Before applying this framework, you should consider the context of your sport and the strength qualities and capacities that your athletes require for success.
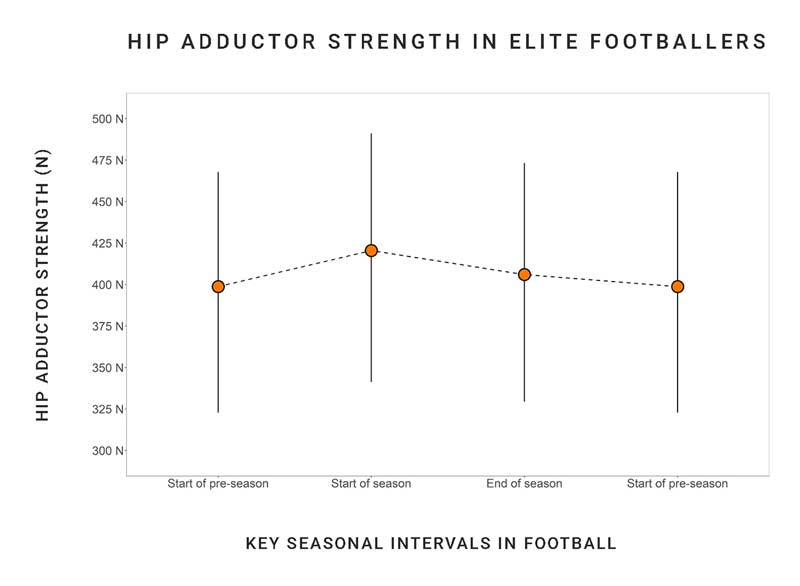
Best practice would be to establish baseline strength data and perform an internal reliability test using a strength testing apparatus such as the ForceFrame from VALD Performance. O’Brien et al.13 has provided a great overview in this paper of validity and normative values in males athletes using the ForceFrame. Baselines can be leveraged to monitor individuals or groups and easily detect any minimal changes in lower body strength. A recent report from VALD Performance demonstrated hip adduction normative values for European football players across a longitudinal period (figure 7), which is often used by practitioners to understand and compare baselines across their athlete cohort.
Performing a groin squeeze is a useful way to monitor pain levels and strength decrements that may persist following a match. It is important to determine what constitutes a meaningful change per athlete, per test—this paper from Thornton et al. provides a great overview of different strategies to determine what constitutes a meaningful change.10One example would be to visualize an athlete’s mean score +/- 1 standard deviation on a longitudinal graph. By viewing the data longitudinally (as seen below in figure 8), you can understand the athlete’s normal response to training and game stimuli.
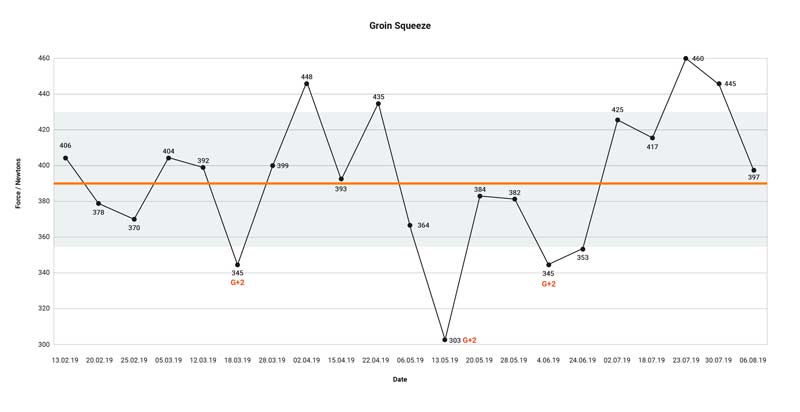
As demonstrated on the above graph, this athlete had three instances where strength levels dropped below their normal variance. If associated with pain or a performance decrement, it would be important to follow up with a physical examination and/or an intervention; the latter may be manual or exercise therapy.
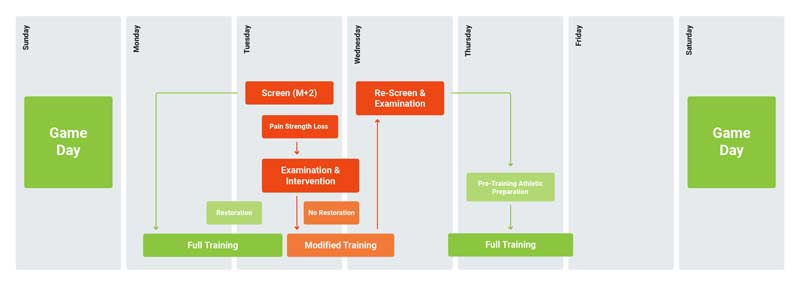
The most important component is to reassess and determine whether there has been a positive change to the strength levels of the athlete, which means they would continue to train, or if there is still residual strength loss. If there has been strength loss, a decision will need to be made on whether the athlete requires a modified training load and strength exercise prescription. An example of how this monitoring protocol based on the framework from Wollin et al. would be implemented for a six-day turnaround in field-based sports can be found below (figure 9):
Example Case Study: Iliopsoas-Related Groin Pain
The following case study depicts a multi-phase return to play strategy, which aims to highlight various strength and monitoring methods that can be used to help athletes successfully return to game demands.
-
Athlete
28-year-old male football (soccer) athlete
History
Gradual onset lower abdominal and right anterior hip pain. Pain usually present at the start of a training session but decreases once “warmed up”; some discomfort with kicking long. Pain increases post training session for approximately 24-48 hours.
Examination
Palpation pain over anterior thigh/lower abdomen. Pain provocation on resisted right hip flexion VAS 5/10 with crossover sign and resisted sit up VAS 6/10. Hip flexor range of motion slightly restricted on right compared to left with some discomfort. Right hip internal rotation restricted but no pain with FADIR; bent knee fallout clear.
Manual therapy able to improve hip flexor range of motion and increase hip internal rotation. Pain decreased but still present with hip flexion 3/10 and sit up 4/10.
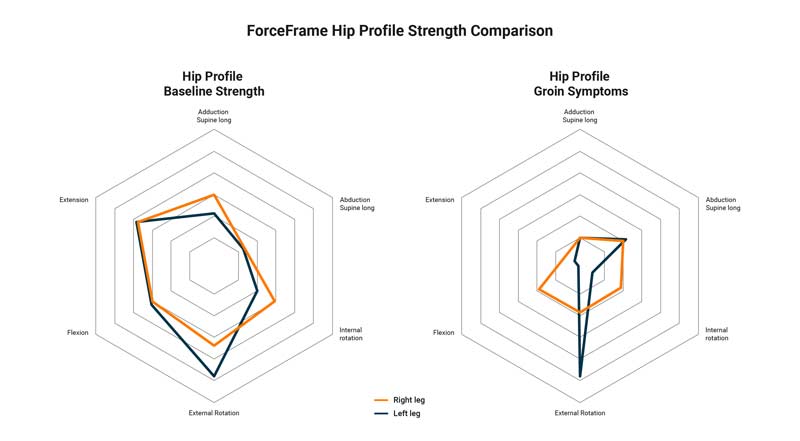
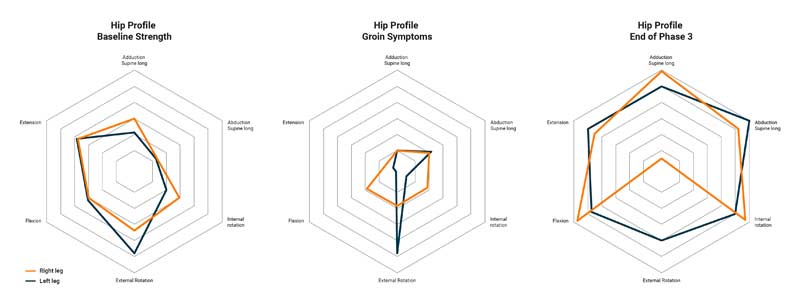
Hip profile strength testing was performed to assess any further strength deficits that may have occurred due to the onset of groin pain and decrement of performance. Figures 10a and 10b illustrate the difference in hip profile strength following the athlete’s presentation of symptoms—a significant reduction in hip flexion, extension, and adduction strength was found in comparison to previous baseline data.
Given the symptoms, palpation tenderness, resisted hip flexion pain, and strength loss, the athlete was diagnosed with iliopsoas-related groin pain as per the Doha agreement guidelines. Due to the severity of pain, performance decrement, and strength loss, the decision was made to stop the athlete from running and kicking and to proceed with conservative management. The key components that were identified as having to be addressed during the reconditioning process were:
- Decrease hip flexion pain.
- Improve hip extension range of motion.
- Improve hip flexion, extension, and adduction strength.
These key components helped create the framework for development of a criterion-based reconditioning strategy for the athlete, which was broken down into four main phases, as listed below.
Phase 1:
This initial phase focuses on hip profile strength accumulation and movement competency. A low level of pain is allowed during this phase of exercise, with the recommendation being below 3/10 on the visual analog pain scale (VAS). Another important consideration is load modification; removing running and kicking addresses the most pain provocative movements and reduces the load on the tissue to allow for strength accumulation. Some running drills can be used to maintain low-level stimulus on lower limb muscle and tendon structures, which can act as a bridge for the athlete to return to run progressions.
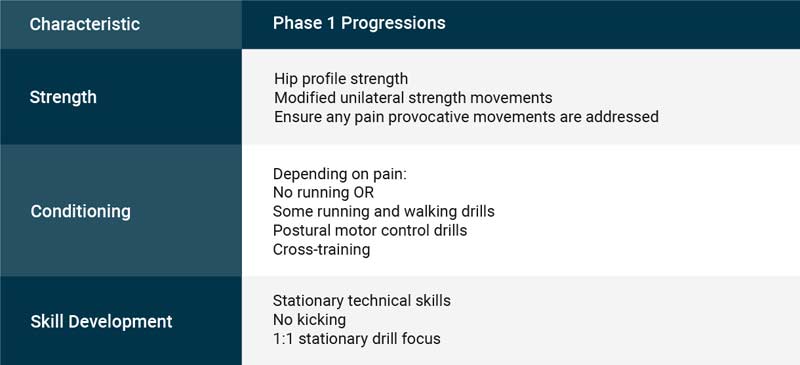
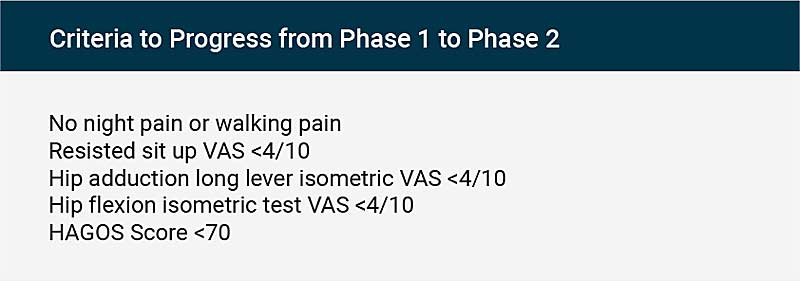
Progressing to phase 2 will depend on findings from the athlete’s presentation and clinical examinations. Using both the HAGOS score and ForceFrame, practitioners can objectively assess hip profile strength and create an individualized exercise prescription.
Phase 2:
The time taken to achieve phase 1 criteria will heavily dictate how quickly you can progress the reloading of linear-based running. The longer an athlete is unable to run, the slower their progression back to normal sessions and weekly volumes will be. This paper11 investigated the impact of workloads on subsequent injury. Further contributions from Matt Taberner on the control-chaos continuum12 also demonstrate how practitioners can interlink the progression of GPS variables while simultaneously increasing perceptual and cognitive challenges throughout the rehabilitation process.
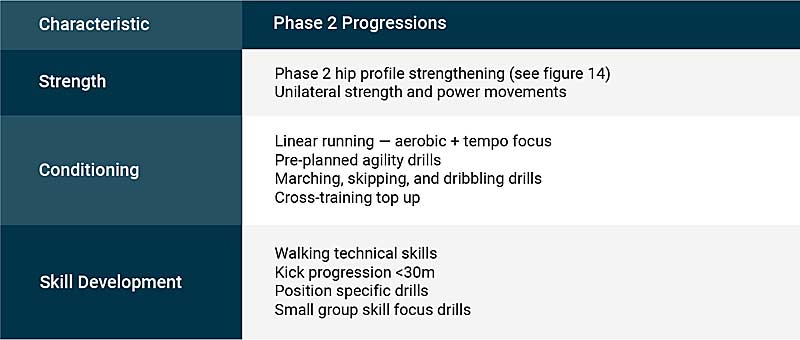
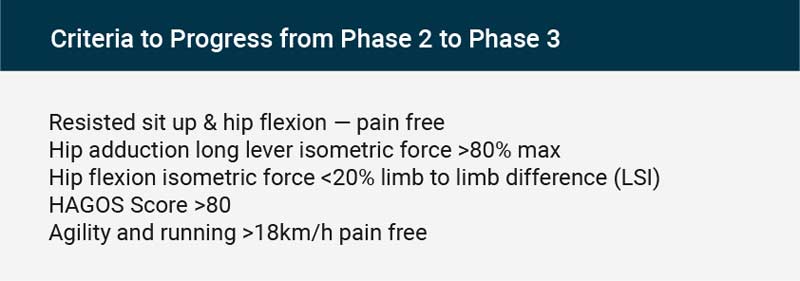
During phase 2, individualized strength exercise prescription (refer to figure 13) is determined based on the athlete’s strength profiling and their strength improvements. Linear running and agility intensity and complexity will progress as comfort allows. Integrating skill- and technical-based development with the assistance of sport coaches is another important consideration for practitioners in this phase, as it provides a good link to the skill integration that follows in phase 3.

Improvements in hip flexion, adduction, and extension strength should continue, and the progress of this is easily measured by the ForceFrame. Pain provocative movements, such as agility and running, should begin to feel comfortable for the athlete.
Phase 3:
The priority in this phase is the athlete’s reintegration into team skills, leveraging both the technical and tactical components of team training to condition the athlete. Monitoring strength and exercise prescription progress during this phase is pivotal, as it helps the athlete in building tissue resilience that will withstand the increased loads of high-intensity running and agility. Individualized conditioning can also be supplemented to build training volumes as required. Skill and technical developments can continue as per phase 2 of team reintegration.
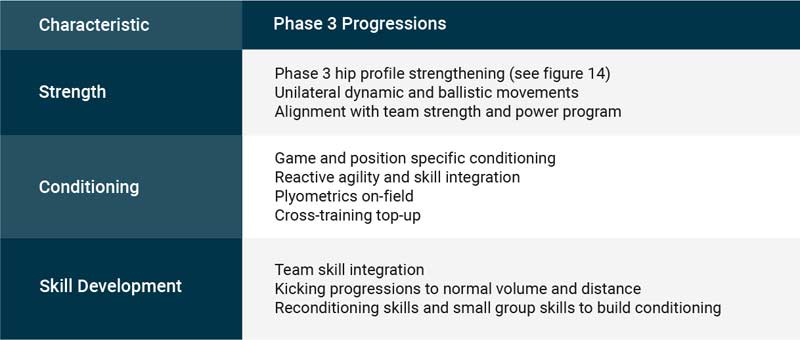
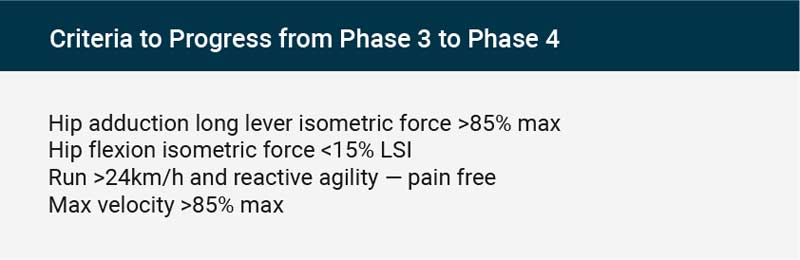
End of phase 3 criteria should see the athlete maintaining hip profile strength, as measured on the ForceFrame. This strength will help guide running speed and agility progressions, all of which they should perform pain free.
Figures 18a-18c below illustrate the change in strength from pre-groin symptoms to the end of phase 3, which shows large improvements in all hip profile strength measurements for both limbs. Interestingly, the athlete demonstrated a decrease in external rotation strength when compared limb to limb, but following further assessment of previous raw values, the right leg external rotation strength was within the athlete’s normal variance.
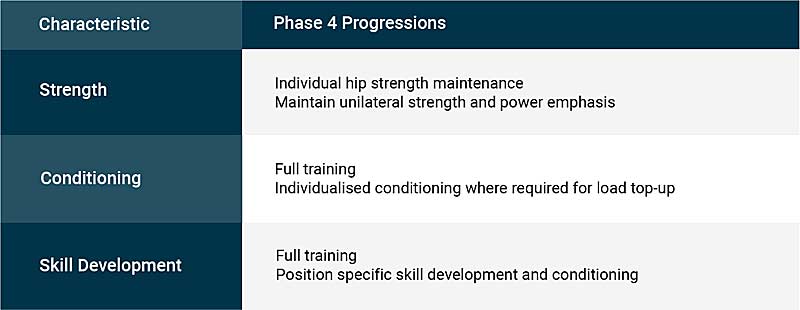
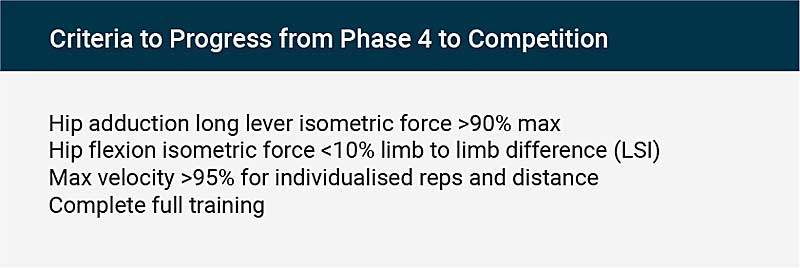
The fourth phase is the most important assessment of the athlete’s physical capacities to determine their return to peak performance and competition. During this phase, it is important to assess how the athlete responds to increases in running intensity, agility, and skill integration. Exposure to adequate training loads, maximum-velocity running, and full contact training is essential for the successful return from injury. Not only should the athlete experience all conditioning progressions pain free, they should maintain individualized hip strength protocols. These should align with regular lower body strength and power exposures, as all will assist with tissue resilience and continued adaptation to training and game loads.
Conclusion
Hip and groin injuries in football athletes are a common occurrence. Most cases are complex and multifaceted, which highlights the importance of an athlete’s management and rehabilitation plan. The development of a comprehensive monitoring framework is important to inform individual variations to training and game stimuli. The combination of a thorough clinical examination as guided by the Doha agreement and hip strength testing using tools such as the ForceFrame is pivotal to inform practitioners and guide key decision-making processes during multi-stage rehabilitation of hip and groin pain.
Since you’re here…
…we have a small favor to ask. More people are reading SimpliFaster than ever, and each week we bring you compelling content from coaches, sport scientists, and physiotherapists who are devoted to building better athletes. Please take a moment to share the articles on social media, engage the authors with questions and comments below, and link to articles when appropriate if you have a blog or participate on forums of related topics. — SF
References
1. Werner, J., Hägglund, M., Ekstrand, J., and Waldén, M. “Hip and groin time-loss injuries decreased slightly but injury burden remained constant in mens professional football: the 15-year prospective UEFA Elite Club Injury Study.” British Journal of Sports Medicine. 2019;53(9):539-546.
2. Weir, A., et al. “Doha agreement meeting on terminology and definitions in groin pain in athletes.” British Journal of Sports Medicine. 2015;49(12):768-774.
3. Falvey, É. C., King, E., Kinsella, S., and Franklyn-Miller, A. “Athletic groin pain (part 1): a prospective anatomical diagnosis of 382 patients—clinical findings, MRI findings and patient-reported outcome measures at baseline.” British Journal of Sports Medicine. 2016;50(7):423-430.
4. Waldén, M., Hägglund, M., and Ekstrand, J. “The epidemiology of groin injury in senior football: a systematic review of prospective studies.” British Journal of Sports Medicine. 2015;49(12):792-797.
5. Orchard, J. W., Seward, H., and Orchard, J. J. “Results of 2 decades of injury surveillance and public release of data in the Australian Football League.” The American Journal of Sports Medicine. 2013;41(4):734-741.
6. Thorborg, K., et al. “Clinical examination, diagnostic imaging, and testing of athletes with groin pain: an evidence-based approach to effective management.” Journal of Orthopaedic & Sports Physical Therapy. 2018;48(4):239-249.
7. Serner, A., et al. “Mechanisms of acute adductor longus injuries in male football players: a systematic visual video analysis.” British Journal of Sports Medicine. 2019;53(3): 158-164.
8. Wollin M, et al. “In-season monitoring of hip and groin strength, health and function in elite youth soccer: Implementing an early detection and management strategy over two consecutive seasons.” Journal of Science and Medicine in Sport. 2018;21(10):988-993.
9. Oliveras, R., et al. “Field-based evaluation of hip adductor and abductor strength in professional male ice hockey players: Reference values and influencing factors.” Physical Therapy in Sport. 2020;43:204-209.
10. Thornton, H., Delaney, J., Duthie, G., and Dascombe, B. “Developing Athlete Monitoring Systems in Team Sports: Data Analysis and Visualization.” International Journal of Sports Physiology and Performance. 2019;14(6):698-705.
11. Stares, J., Dawson, B., Peeling, P., Drew, M., Heasman, J., Rogalski, B., and Colby, M. “How much is enough in rehabilitation? High running workloads following lower limb muscle injury delay return to play but protect against subsequent injury.” Journal of Science and Medicine in Sport. 2018;21(10):1019-1024.
12. Taberner, M., Allen, T., and Cohen, D. “Progressing rehabilitation after injury: Consider the ‘control-chaos continuum’.” British Journal of Sports Medicine. 2019;53(18)1132-1136. bjsports-2018. 10.1136/bjsports-2018-100157.
13. O’Brien, M., Bourne, M. N., Heerey, J., Timmins, R. G., & Pizzari, T. (2019). “A novel device to assess hip strength: Concurrent validity and normative values in male athletes” [accepted manuscript].





