[mashshare]
Omega-3s are riding an alpha wave of hype. In the sports world, the use of omega-3s as a nutraceutical for repetitive head trauma and concussions is gaining momentum. This escalated demand, combined with a minimal consumption of fish and multiple studies reporting alarming omega-3 deficiencies among athletes and the general population, creates a perfect storm for supplement companies to swoop in and take advantage by marketing high-priced omega-3s.
Unfortunately, there’s confusion over which omega-3 product to purchase, which results in many puzzled looks when facing an overwhelming selection of omega-3 supplements in the vitamin aisle. Additionally, most supplement dosages don’t even match the research, and this makes efficacy highly questionable. After all, who wants to gulp down 10 fish oil pills each day?
While everyone is so concerned with omega-3 supplementation due to omega-3 deficiencies and the consequences of those deficiencies, very little attention is being given to the molecular carrier of the omega-3. This carrier heavily influences bioavailability, retention in the body, and subsequent efficacy in improving omega-3 deficiency to obtain desirable health outcomes. If the goal is a quick and efficient recovery from DHA deficiency, then the different forms of DHA supplementation must be considered.
This perfect storm of formula problems suggests omega-3 supplements are overpriced and overhyped. If you’re looking for more value than the nonchalant “just take an omega-3 supplement,” this article will tell you how to find a valuable source of omega-3s to better exploit their nutritional properties.
What Are Omega-3s?
Omega-3 polyunsaturated fatty acids are essential fatty acids (we must get them from the diet) that are critical for normal cell growth and development.
The main omega-3s are:
- Docosahexaenoic Acid (DHA): A long-chain fatty acid that is needed to create neuronal synapses (i.e., where signaling occurs for cell-to-cell communication) and membrane fluidity. Every cell in the body contains DHA, but it is mostly concentrated in the eyes (93%) and brain (97%), especially in areas involved in memory and attention.
- Eicosapentaenoic Acid (EPA): A long-chain omega-3 needed for overall health.
- Alpha-Linolenic Acid (ALA): A short-chain omega-3 that serves as an energy source and building block for DHA and EPA. We must directly increase DHA intake because the conversion of ALA to EPA is 8% and then from EPA to DHA is 0-4%. So, ALA is not sufficient for increasing DHA in the brain.
DHA and EPA are structural components of cells, while ALA is used more as an energy source. DHA and EPA deliver critical biological effects, such as fighting inflammation and providing cardiovascular benefits. Low levels of DHA in the brain or eyes can slow down signaling (communication) between cells, which leads to poor vision and weaker cognition (e.g., development of learning, reaction time, etc.).
Read more about DHA here.
The Hierarchy of Factors to Consider in Omega-3 Efficacy
To obtain the benefits of omega-3s that have been extensively reported, sufficient intake and duration of intake, as well as transport and assimilation into brain and blood cells are all key. DHA comes in the form of food or supplement from cold-water fish (such as salmon, mackerel, herring, and tuna), algae, and Antarctic krill.
Just because you take in a certain nutrient doesn’t mean that you will digest all of it. Share on XBefore someone can argue about the efficacy of any supplement, there is a hierarchy of factors to consider:
- Dosage: The amount of DHA/EPA in the food or supplement.
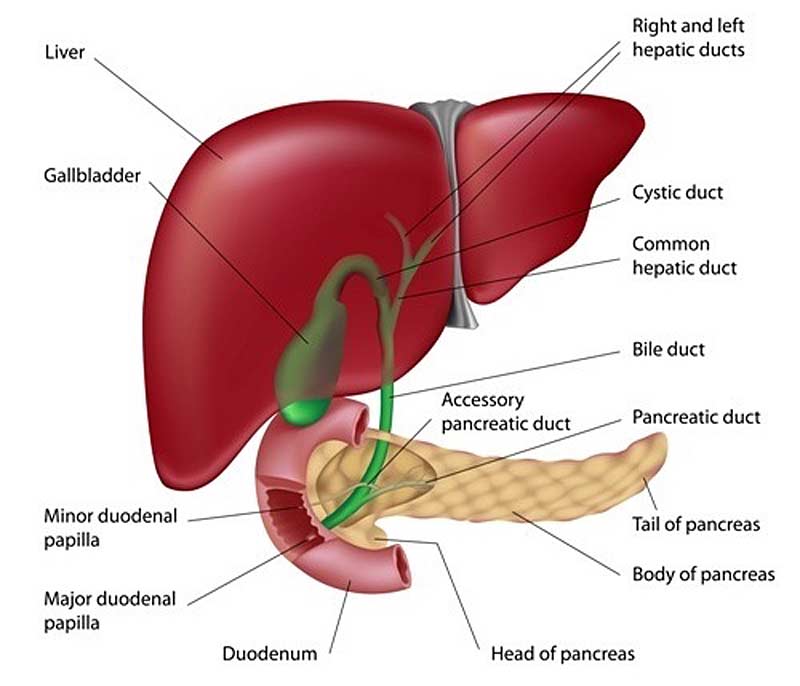
- Bioavailability: Think of this as the amount of a nutrient consumed and how digestible the nutrient is. Just because you take in a certain nutrient doesn’t mean that you will digest all of it. For dietary fat digestion, enzymes are used in the hydrolysis of fat in the small intestine. Then, the hydrolyzed by-products are absorbed across the gut lining. Essentially, bioavailability describes how much of a nutrient is taken in and actually retained in the body fat through digestion and absorption.
- Absorption: After digestion, micelles transport the fatty acids to the surface of the gut lining, where they can be absorbed.
- Metabolic Fate/Retention in Tissue: Metabolic fate is where the omega-3s go after digestion and absorption. Omega-3s need to get into circulation and then assimilate into compartments in the body, such as red blood cells (RBC), adipose tissue, muscle, and brain.
Essentially, not all omega-3s from food and supplements are the same with respect to bioavailability, absorption, and metabolic fate. Why is this so? Because omega-3s contain differences in chemical form (or carriers) when they come from food versus when they come from supplements. This is the reason omega-3 research regarding health outcomes is unclear and mixed results have been reported: It’s not an equal playing field when comparing foods and supplements.
The efficiency of the omega-3 carrier studied in the research is rarely focused on. Subsequently, a majority of supplement companies do not ensure that the omega-3 carrier in their omega-3 source is sufficient for bioavailability. In the research using omega-3 supplements, minimal attention has been given to the bioavailability of omega-3s in different dietary supplements. This major oversight impacts absorption and metabolic fate as well.
It’s interesting that of the large number of publications researching the biological and health effects of omega-3s, very few studies directly focus on omega-3 bioavailability. This is the reason it’s considered almost impossible to compare the outcomes of the studies1—there are so many differences, including the study design, number and sex of participants, duration of studies, different carriers of omega-3s, different measures used to estimate bioavailability, and more.
Ultimately, it is evident that the carrier of the omega-3 affects its bioavailability and subsequent efficacy.
Different Molecular Carriers of Omega-3s
In nature, omega-3 fatty acids (FA) are found in triacylglycerol (TAG)/triglyceride (TG), phospholipid (PL), or free fatty acid (FFA) form. Most omega-3s from fish are found in the TG form, which is considered the “natural” form. Fish oil comes from fish that are processed and encapsulated into supplements. Omega-3s can also be converted into other forms, such as ethyl ester (EE), which is an oil concentrate.
Preformed DHA is considered structurally identical, but in food and supplements, DHA typically undergoes an enzymatic and chemical reaction (or is esterified) to become one of four different lipids that serve as molecular carriers:
- Triacylglycerol/Triglycerides: Consists of three fatty acids connected to a glycerol backbone. This form of lipid is found in foods like fish, seafood, and fish oils. There are small amounts of monoacylglycerol (MAG), diacylglycerol (DAG), or phospholipid (PL) in foods.
- Phospholipid: Consists of two fatty acids connected to a glycerol backbone and a phosphorous group that is linked to a “head group,” which consists of choline, ethanolamine, and other types of phospholipids. So instead of a third fatty acid, there’s a phosphate or choline added. Of the forms of PL, one of the most important forms is DHA-enriched phosphatidylcholine (DHA-PC), which is the most predominant PL in salmon, tuna, rainbow trout, and mackerel. An important PL is lysophosphatidylcholine (lyso-PC), which is discussed further below.
- Free Fatty Acid: These aren’t connected to a glycerol backbone; hence, “free” fatty acid.
- Ethyl Ester: The synthetic form, where DHA/EPA is connected to ethanol, which produces an omega-3 oil concentrate.
Cold-water oily fish, such as salmon, sardine, anchovy, herring, and mackerel, contain between 1-1.5% PL and 10-15% TG.2Up to 33% of the EPA and DHA may be in the form of PL, depending on the type of fish.3The FA content is different in farmed fish compared to wild fish because of the aquaculture feed.
Does esterifying the omega-3 source in TG or PL form influence absorption efficiency of FAs into the blood? Does this impact the subsequent effects on integration into tissue and long-term health outcomes?
Metabolism of Omega-3s
The metabolism of omega-3s is highly important in evaluating bioavailability and retention in the body and will be briefly described.
In our gastrointestinal tract, the TGs are broken down into FFAs and MAGs. They are then absorbed by our gut cells, put back together to form TAG, and transported in chylomicrons (small globules that transport fat) to the liver. There, the FAs are either stored in the liver or exported in very low-density lipoprotein to target tissues like muscle, adipose, red blood cell (RBC), brain, etc., where they are usually incorporated in membranes.
DHA is rapidly sent to:
- Plasma Lipoproteins– Mostly as TG or PL.
- Blood– As non-esterified DHA or lysophosphatidylcholine-esterified DHA (lysoPC-DHA).
Studies suggest that DHA bioavailability to the brain is greater when DHA is in the lysoPC-DHA form in the blood even though non-esterified DHA is still a good source of DHA.4-7But how DHA enters the brain is still a mystery. The preferential crossing of the blood-brain barrier in the lysoPC-DHA form is supported by a few studies, which is further supported by the finding of a specific transporter of lysoPC-DHA called MFSD2A (major facilitating superfamily domain-containing protein 2A).
The other important factor is that DHA in the lysophospholipid form has a longer plasma half-life, which increases DHA brain exposure. This has important implications for brain diseases.
Phospholipids are digested and absorbed differently than TAGs. It’s a bit more complicated. Phospholipids enter the hepatic system as micelles (a stable group that is essential for fat absorption), so they’re more bioavailable.
Evaluation Process of Omega-3 Status
Aside from digestion, absorption, and transport, omega-3 retention and incorporation into tissue are endpoints to be considered. Long-term studies (multiple weeks or months) determine omega-3 status by examining the levels in RBCs, which are suggested to closely parallel DHA levels in the brain.8Omega-3 status determined via RBCs is thought to reflect long-term availability.
The Omega-3 Index is valuable, but it’s only part of my evaluation process for omega-3 status. Share on XMany studies have shown that the concentration of EPA and DHA in RBC membranes correlates well with omega-3 levels in cell membranes of other tissues like the heart, liver, and brain.9-11Specifically, the omega-3 index—the total of EPA and DHA presented as a percentage of total FA in RBC membranes—is a sufficient measure of long-term incorporation of FA in tissue.

For example, the Omega-3 Index, along with other tests, was critical in holistically evaluating that one of my NFL players was not getting enough omega-3s in his food-first approach, despite consuming multiple servings of salmon per week. Therefore, we re-strategized in our goal to increase brain resilience by following a nutrition-first approach instead of only a food-first approach.
The Omega-3 Index is valuable, but it’s only part of my evaluation process for omega-3 status.
Factors Impacting Bioavailability of Omega-3 Carriers
For omega-3s, think of bioavailability as the dosage of EPA/DHA that you consume and the number of these FAs that raise the amount of omega-3s in your blood. When it comes to DHA and EPA, we need to make sure that the type of fat carrying these critical nutrients provides high bioavailability. Otherwise, impaired absorption is worthless, especially at the price of $1+ per serving of fish oil.
Omega-3 dosage and bioavailability are critical factors before we can completely disregard omega-3s for specific health and performance benefits (e.g., reaction time, brain resilience, etc.).
Long-term and short-term studies are complementary in understanding omega-3 bioavailability and their biological effects.
- Long-Term Studies: Provide the bioavailability and subsequent metabolic fate, which is more informative about the biological effects of omega-3s.
- Short-Term Studies: Better for evaluating the bioavailability of omega-3s, but not information about metabolic fate and accumulation in tissue.
In actuality, studies investigating bioavailability should consider supplementation over an extended period of time instead of a single dose in order to be certain.
Much of the discrepancy between studies can be correlated to variables such as different levels of EPA and DHA, different treatment times (a few days versus eight weeks), and different doses used (e.g., 3 grams versus 2 grams).
It is difficult to analyze bioavailability when studies make gram-for-gram comparisons of different omega-3 carriers: for example, 2 grams of an omega-3 supplement in the PL form versus 2 grams of an omega-3 supplement in the TG form. It is suggested this is inappropriate and could lead to inaccurate results. Bioavailability determines efficacy even in the comparison of identical dosages of omega-3s of two different forms.
Another two factors to consider are the food matrix that influences the bioavailability of the nutrients in it and the total dietary fat consumed with omega-3 supplements (e.g., consuming an omega-3 supplement that contains eggs and avocado at breakfast). Significant effects on omega-3 bioavailability are related to the amount of dietary fat. A high-fat meal significantly improved absorption of the EE and TG forms in humans when compared to a low-fat meal (44 grams of fat versus 8 grams of fat). There’s a higher omega-3 bioavailability if you consume omega-3s with a high-fat meal.
There’s a higher omega-3 bioavailability if you consume omega-3s with a high-fat meal. Share on XThen there’s the influence of formulations that focus on improving tolerance and/or increasing bioavailability. An emulsified form may provide higher availability, which may lead to better digestion and absorption of omega-3s.12Microencapsulated fish oil compared to fish oil capsules may also enhance bioavailability, possibly due to easier breakdown. However, enteric coating, which is resistant to stomach acidity, is suggested to have no influence on bioavailability.13,14
Bioavailability Comparison of Different Omega-3 Carriers
First and foremost, TG is considered more effective than EE. DHA in natural fish oil is typically esterified to TG and PL. But, if the form impacts the bioavailability, does the form also influence where the omega-3, specifically DHA, is incorporated in the body (e.g., the brain or RBC)? It is suggested that DHA-PC could increase DHA in RBCs better than DHA-TG.15
Studies using PL versus TG showed significantly greater incorporation of omega-3s into tissues from PL compared to TG. Of the PL forms, PC is a highly efficacious source for DHA. A study has shown that the metabolic fate of DHA differs quite a bit when taken in as TG compared to PC for bioavailability of DHA in plasma and storage in various tissues in the body.
Multiple studies have shown that DHA-PC results in a higher bioavailability and greater efficacy of accumulation in the brain compared to DHA-TG.15,16 With respect to outcomes, DHA-PC has produced more significant improvements in cognitive performance and emotional well-being compared to DHA-TG.
A study investigated the efficacy of dietary DHA carried by PC compared to DHA carried by TG in pigs.15Researchers found that dietary DHA carried as PC is more efficient at being incorporated as brain gray matter DHA than DHA carried as TG. It was also more effective in the retina, liver, and red blood cells.
It’s important to note that DHA is in the phospholipid form in the cell membranes of the brain and retina. This includes phosphatidylcholine and phosphatidylserine.
A 2018 study assessed the bioavailability of different DHA carriers by comparing the incorporation of DHA in plasma, RBCs, retina, and brain tissues in adult rats provided with PL-DHA or MAG-DHA over 60 days. To evaluate the PL and MAG carriers, they were compared to DHA oil containing the usual TG-DHA.
The study found that MAG-DHA and PL-DHA are more efficient than TG-DHA in increasing DHA levels in RBCs. The study reported that PL-DHA enriched oil may require minimal digestion before absorption, which is a key factor in omega-3 efficacy.
Ultimately, the differences were assumed to be due to absorption, and if most fish oil supplements are TG-bound, then this is an important issue due to dietary PL consistently showing better bioavailability. Essentially, in PL versus TG, human studies do not have conclusive results, but animal studies suggest the PL form may improve the bioavailability of omega-3s, which helps enhance absorption of EPA/DHA.
This carrier may be important if the goal is brain resilience because the key is DHA accumulation kinetics in the brain. Lowering the DHA concentration in the liver could be helpful for increasing DHA availability for other tissues.15 This could be done by providing DHA as PL rather than as TG for building up brain DHA.
Gut Microbiota Implicated in Omega-3 Absorption
Gut microbiota are suspects in the bioavailability issue. The latest research suggests that some gut microbiota could be snatching the omega-3s. When TAGs are digested, a portion of the free fatty acids released may be used as a carbon source (i.e., energy source) for our gut microbiota, and the leftovers may be eliminated in our feces. This means the >$1 price per serving on your probiotic supplement may be feeding your gut microbiota more than depositing DHA in the brain to increase brain resilience.
Your probiotic supplement may be feeding your gut microbiota, not depositing DHA in the brain. Share on XThe interesting part of the 2018 study described above is that the researchers discuss a novel, hypothetical mechanism as to why there is a difference among the carriers leading to differences in the amount of DHA circulating in the body. It was suggested that part of the FFAs released from TAG are neither absorbed nor excreted. So where do they go?
They were taken up by the gut microbiota. Some bacteria, such as Lactobacillaceae, can metabolize FAs. Therefore, it is suggested that some of the FFAs released from TAG can be used by gut microbiota. It’s estimated that gut microbiota use 5-15% of the FFAs released from TAG.
After TAG is broken down into MAGs and FFAs, they can enter one of three different pathways:
- Chylomicron Synthesis: absorption into fat globules used for transportation
- Excretion: in our feces
- Gut Microbiota: uptake and use for energy
It is estimated that the resulting differences in absorption leads to:
- 80-90% of total FAs absorbed from TAG
- 0-5% of FFAs are excreted in our waste
- 5-15% of FFAs are used by the gut microbiota
Essentially, it appears that MAG-DHA and PL-DHA are more efficient at increasing DHA levels in RBCs compared to TAG-DHA. And the reason for the difference in absorption may be due to our gut microbiota snatching some of the FFA during the digestion of TAG.
Do Omega-3s Really Have an Impact on Brain Resilience?
DHA is recognized as a critical nutrient for brain cell communication with anti-inflammatory effects in the brain, which recommends its use as a strategy for several brain diseases that are inflammatory. Increasing brain DHA may protect from neuroinflammation associated with aging, pro-inflammation, or an acute injury such as a concussion.
Since brain DHA levels depend on diet, bioavailability must be a priority. The function of DHA and its critical role in brain development, cognition, and vision is well-supported. The big issue is understanding how DHA actually accumulates in the eyes and the brain, especially when there is tight regulation in the separation of blood circulation by the blood-brain barrier.
Since brain DHA levels depend on diet, bioavailability must be a priority. Share on XDoes the RBC DHA level serve as a biomarker of DHA accumulation in the brain? The efficacy and incorporation of DHA into tissues in our body is questionable.
The form of PL called lysoPC is suggested (based on young rats) to be the desired vehicle of DHA to the brain compared to TG.8,17LysoPC carrying DHA may increase brain penetration, which would serve as an important factor in the therapeutic treatment of neuroinflammation.
The bottom line: We tout the value of increasing DHA in the brain, but we don’t yet fully understand the different forms that transport the DHA into the brain. The DHA carrier is highly important.
Dosage: Intake vs. Uptake
Different national and international health authorities recommend omega-3 intakes that range from 250 milligrams per day to up to 2 grams per day of EPA and DHA. Remember, what is on the label doesn’t really translate to what is in the body.
Research suggests that dosage not be provided as a fixed amount, but rather, based on body weight.1For example, consider 1 gram of EPA in TG given to two different people, one who weighs 60 kilograms and another weighing 90 kilograms. Although the 60-kilogram person receives a dose that is 50% less than the 90-kg person, as their weight is 50% less as well, the doses aren’t equivalent as compared to bodyweight. In this scenario, one dose is equivalent to 0.0017% of body weight for the 60-kg person, and 0.0011% of body weight for the 90-kg person. This results in variability in the omega-3 status measurement assessing bioavailability.
A systematic review also showed that women have a significantly higher amount of DHA in their plasma/serum, RBC, and adipose tissue compared to men. Therefore, sex plays a role in omega-3 bioavailability as well.
Additionally, initial nutritional status may influence the efficiency of recovering DHA depletion, which requires a different dosage. What is the key dosage? Well, that depends.
Note that dosage is your intake, but your uptake is a different ball game.
When Dosage Is Really a Problem
Omega-3 supplements are a promising nutritional approach for optimizing brain health, especially related to cognition and warding off neurological diseases. But with the information above, the evidence suggests that omega-3 supplements are definitely not all equal. Given the need for therapeutic use, two populations for whom dosage is a major concern are:
- Athletes of Collision Sports: For football, hockey, rugby, etc., a high dosage and efficacy is key to potentially alleviate long-term consequences related to the brain and neuroendocrine system. Supplement companies are jumping on the bandwagon and claiming that their product can be a preventative nutraceutical. Unfortunately, many do not have dosages that match the literature. Where are the bioavailability studies that are especially well-controlled? Is there a formulation issue?
- Carriers of the Apolipoprotein E e4 Allele: Chronic high doses of DHA to those who carry the APOE4 allele may reduce the risk for Alzheimer’s Disease (AD). APOE4 is one of three forms of APOE that lead to an increased risk for AD, such as less-effective clearance of B-amyloid plaque that causes cognitive decline, higher inflammatory response, and lower ability to cope with the consequences of brain injury. Those with one e4 allele have three to four times the risk of developing Alzheimer’s compared to those without the allele. However, this nutrient timing needs to happen before the onset of dementia. It is suggested that APOE4 is a modifiable AD risk factor and DHA supplementation may help alleviate the neurological disease. It’s a perfect storm for an athlete who has this gene and is playing a collision sport.
Practical Advice
After reading this article, you’re probably thinking: So what? The purpose of this article was not to confuse people, but rather to pose questions that determining omega-3 supplementation for different biological effects is not easy. It’s not just about “take a supplement.”
The issue boils down to the fact that omega-3 supplements vary in dosage and the type of dietary carrier used, which influences the incorporation of DHA into tissue. Just because you’re taking an omega-3 supplement for brain health, doesn’t mean that it’s going straight to the brain. The variables, such as the omega-3 carrier, that influence the ability of DHA to get into the brain need to be optimized.
If different forms of omega-3s have different bioavailability profiles, do we need to aggressively vet omega-3 supplement companies? What are the bioavailability claims of omega-3 supplement companies, or are they brushing that variable to the side?
Dosage is obviously a critical factor when determining which omega-3 supplement to provide. Unfortunately, the majority of omega-3 supplements are not formulated with dosages that match the literature for efficacy. Therefore, we’re battling dosage issues combined with poor bioavailability.
When unknowingly facing misleading or false claims from omega-3 supplement companies, how can you optimize your omega-3 intake? The difficulty with supplement companies is that many do not disclose an important component on the label: the specific form of EPA or DHA used. This makes it challenging for the consumer to compare omega-3s.
Additionally, some companies add “label dressing.” Maybe a stack of vitamin D and omega-3 makes sense, but the addition of other components like MCT oil is unnecessary.
The transparency for omega-3 supplements appears non-existent.
Should you just stick to food? The amount of EPA/DHA in salmon ranges from 999 to 1,825 milligrams per 3-ounce serving. But how many people are consistently eating salmon at least two times per week? And does a food-first approach allow for therapeutic dosages to be reached?
A study that compared 600 milligrams of DHA from algae oil to cooked salmon over a two-week period found that the two were bioequivalent in nutritional availability. This is where I stick to a nutrition-first approach: Consume omega-3s from food, but also supplement. Use blood testing to figure out the dosage need for that individual person.
Re-Think Omega-3 Supplements
Omega-3s are a more complex process than what may be admitted, which makes them subject to a lot of variability when evaluating their preventative and therapeutic benefits, especially for concussion. Efficacy boils down to dosage, bioavailability, absorption, and incorporation into different tissues and organs of the body.
Omega-3 supplements can be a big expense in your arsenal of supplementation. “Sexy” omega-3 bottle labels mask bioavailability issues, and many of these supplements may not be adding any nutritional value because their bioavailability isn’t completely there.
Omega-3 supplementation is warranted—pay attention to intake and the variables impacting uptake. Share on XWithout a doubt, omega-3 supplementation is warranted. Focus on the intake and variables impacting uptake. Hopefully, omega-3 supplement companies will catch on that providing value that translates into future health benefits starts with the right formulation.
Since you’re here…
…we have a small favor to ask. More people are reading SimpliFaster than ever, and each week we bring you compelling content from coaches, sport scientists, and physiotherapists who are devoted to building better athletes. Please take a moment to share the articles on social media, engage the authors with questions and comments below, and link to articles when appropriate if you have a blog or participate on forums of related topics. — SF
[mashshare]
References
- Ghasemifard S, Turchini GM & Sinclair AJ. “Omega-3 long chain fatty acid ‘bioavailability’: a review of evidence and methodological considerations.” Prog Lipid Res. 2014; 56:92-108.
- Hjaltason B & Haraldsson GG. “Fish Oils and Lipids from Marine Sources.” In Modifying Lipids for Use in Food; Gunstone, F.D., Ed.; Woodhead Publishing: Cambridge, UK, 2006; pp.57-79.
- Xu R, Hung JB & German JB “Effects of dietary lipids on the fatty acid composition of triglycerides and phospholipids in tissues of white sturgeon.” Aquacult. Nutr. 1996; 2:101-109.
- Bernoud N, Fenart L, Moliere P, Dehouck MP, Lagarde M, Cecchelli R & Lecerf J. “Preferential transfer of 2-docosahexaenoyl-1-lysophosphatidylcholine through an in vitro blood-brain barrier over unesterified docosahexaenoic acid.” J Neurochem. 1999; 73:338-45.
- Lagarde M, Bernoud N, Brossard N, Lemaitre-Delaunay D, Thies F, Croset M & Lecerf J. “Lysophosphatidylcholine as a preferred carrier form of docosahexaenoic acid to the brain.” J Mol Neurosci. 2001; 16:201-4. Discussion 215-21.
- Picq M, Chen P, Perez M, Michaud M, Vericel E, Guichardant M & Lagarde M. “DHA metabolism: targeting the brain and lipoxygenation.” Mol Neurobiol. 2010; 42:48-51.
- Thies F, Pillon C, Moliere P, Lagarde M & Lecerf J. “Preferential incorporation of sn-2 lysoPC DHA over unexterified DHA in the young rat brain.” Am J Phys. 1994; 267:R1273-9.
- Innis SM. “Plasma and red blood cell fatty acid values as indexes of essential fatty acids in developing organs of infants fed with milk or formulas.” Journal of Pediatrics. 1992; 120(4):78-86.
- Metcalf RG, James MJ, Gibson RA, Edwards JR, Stubberfield J, Stuklis R, Roberts-Thomson K, Young GD & Cleland LG. “Effects of fish-oil supplementation on myocardial fatty acids in humans.” Am J Clin Nutr. 2007; 85:1222-1228.
- Harris WS, Sands SA, Windsor SL, Ali HA, Stevens TL, Magalski A, Porter CB & Borkon AM. “Omega-3 fatty acids in cardiac biopsies from heart transplantation patients: correlation with erythrocytes and response to supplementation.” Circulation. 2004; 110:1645-1649.
- Tu WC, Mühlhäusler BS, Yelland, LN & Gibson RA. “Correlations between blood and tissue omega-3 LCPUFA status following dietary ALA intervention in rats.” Prostaglandins Leukot. Essent. Fatty Acids. 2013; 88:53-60.
- Ikeda I. “Digestion and absorption of structured lipids,” in A.G. Chrisyophe & S. DeVriese (Eds.), Fat Digestion and Absorption, AOCS Press, Champaign, IL, 2000, pp. 235-243.
- Schneider I, Schuchardt JP, Meyer H & Hahn, A. “Effect of gastric acid resistant coating of fish oil capsules on intestinal uptake of eicosapentaenoic acid and docosahexaenoic acid.”J Funct Foods. 2011; 3:129-133.
- Kurowska EM, Dresser GK, Deutsch L, Vachon D & Khalil W. “Bioavailability of omega-3 essential fatty acids from perilla seed oil.” Prostaglandins Leukot. Essent. Fatty Acids. 2003; 68: 207-212.
- Liu L, Bartke N., van Daele H, Lawrence P, Qin X, Park HG & Brenna JT. “Higher efficacy of dietary DHA provided as a phospholipid than as a triglyceride for brain DHA accretion in neonatal piglets.” J Lipid Res. 2014; 55:531-539.
- Ramprasath VR, Eyal I, Zchut S & Jones PJ. “Enhanced increase of omega-3 index in healthy individuals with response to 4-week n-3 fatty acid supplementation from krill oil versus fish oil.” Lipids Health Dis. 2013; 12:178.
- Thies F, Pillon C, Moliere P, Lagarde M & Lecerf J. “Preferential incorporation of sn-2 lysoPC DHA over unesterified DHA in the young rat brain.” American Journal of Physiology. 1994; 267(5):R1273-R1279.



