[mashshare]

If you listed the most common variable in losing a game or a medal, injuries would likely surface more than any coaching error. Next to traumatic brain injuries, muscular or joint injuries are the No. 1 challenge. In sport, injuries to a knee or a pulled muscle are normal and expected, but their rate of occurrence is currently under the microscope. Any progressive team wants to cut back on injuries and reduce rehabilitation time.
In this buyer’s guide, we review the emerging technologies and the current gold standard options to help teams reduce injuries and sometimes even prevent them from occurring. Each monitoring system is unique, meaning the instruments are not interchangeable, but all of them share the ability to help practitioners become more objective. Every system listed is strong enough for research and also clinically friendly, so that they are all fine choices in a demanding team environment.
The Difference Between Function Monitoring and Injury Diagnosis
Diagnosis and function are two distinct terms. Medical imaging solutions like an MRI or X-ray and functional performance with tensiomyography and elastography are different animals. We assume that all readers of this guide are fully aware of the key differences between them.
Functional status—how the tissue responds or performs—is different than injury diagnosis. Injury is more straightforward: the athlete damages part of their body and medical imaging, along with clinical evaluation, reveals the extent of the damage and what the injury is. This is clear with a broken bone or sometimes with a torn muscle when the injury is acute, but chronic pathologies are often more complicated. Functional status is a measure of how the area is working, and sometimes even uninjured athletes have a functional status that is far from ideal. The prevention of injuries is far less simple and clear, as trends in function that may lead to injury require more interpretation. They are only probabilities and possibilities; they are not guaranteed.
Functional status—how the tissue responds or performs—is different than injury diagnosis. Share on XSometimes, overlap of diagnosis and functional status will occur, as most medical imaging requires a radiologist to interpret the images and come to a conclusion. Most imaging of the soft tissue in chronic injuries evaluates the structure and visual status of the injury region, not the performance of the muscle or joint. Functional status could be active field testing, as athlete performance is the end game, but for the most part functional status is either passive or isolated. A clear example is the Nordbord, a system that can be great for athletes at the end of rehab, but is not useful immediately after injury, such as TMG. Other preventive systems are great for showing increasing risk or risk factors, but prediction is a whole different ball of wax, and you should use caution when one metric in isolation reveals a red flag.
Functional, as a term, is very difficult to pin down in sports performance and sports medicine. It used to mean balance or single leg exercises, as several proponents imprinted their definition on the term, but it’s really about how the solution, whether an exercise or approach, helps in achieving results. The old notion is that functional used to mean it visually appears sport-specific—an outdated paradigm—as the new definition is that function really means it’s effective.
What Are Muscle and Joint Function Monitoring Systems?
As mentioned earlier, muscle and joint function monitoring systems are instruments that reveal more information on how the tissue or joint is working (mainly active), rather than just what it looks like (medical imaging). Some systems do use cameras or create images, but they monitor the pattern of function rather than try to diagnose an injury or pathology. While it’s obvious there is some overlap between functional monitoring and medical imaging, the cardinal difference is we use one to monitor and the other sparingly to help reveal possible injury.
Several categories of muscle and joint status exist, and most of the methods test the strength, readiness, and response to stimuli or action.
Muscle Performance: Conventional science considers isolated strength testing, such as isokinetic strength machines, to be functional status with return to play, but since they are training devices, they’re also strength training solutions. Equipment such as dynamometers are more about testing than training.
Soft Tissue Status: Sonography and elastography are medically driven solutions, but new methodologies use conventional medical devices to help measure objective changes to tissue, including fascicle length and the similar.
Neuromuscular Function: Electromyography is more of a research or feedback option, and while we can consider it a monitoring tool with smart fabrics, those solutions belong in a review by themselves. Tensiomyography and myotonography are more about the function of the tissue itself than the activity of the muscle in a movement.
Biological Pattern Monitoring: Thermography is a biological monitoring tool and requires interpretation and cross validation for proper analysis. Core temperature is a research-only tool due to practical limitations and athlete compliance. Thermography is not a fatigue-monitoring tool, but inferences with fatigue are possible with additional data sets.
Overall, the market is wide and other approaches that connect to joints and muscle groups are available. For the most part, however, research doesn’t establish their role enough to even consider them promising. Most of the applications in monitoring joint and muscle function require additional testing or clinical interaction with athletes, and are not summary tools by themselves. Objective and repeated use are two of the most important characteristics of the systems, and every option ranges from very passive to highly active.
The Spectrum and Technologies That Evaluate Tissue and Joint Function
The key spectrum with monitoring options is the width of data and the passivity of the information. When monitoring joints and muscle groups, most teams and staff want measures that don’t require athlete effort, as field testing might create residual fatigue and require athlete motivation. Most tests need to isolate specific and very narrow qualities or characteristics of joints and muscles, and field tests can sometimes hide poor function.
Athletes are great compensators and often mask low-level injuries that can grow and worsen over time. Some systems, like algometers, use pressure to quantify pain, but we don’t include anything perceptual in this review as they are subjective measures. We recommend clinical experience and athlete or patient feedback, but again, the equipment in this guide does not measure it.
When looking at muscle function, the spectrum starts with readiness and then progresses to performance. Fatigue is nearly impossible to assess, but you can see the collateral effects of heavy training with many of the instruments listed below.
Readiness: While a body’s freshness and sharpness does seem like a prediction of performance, for the most part, fatigue requires several metrics to estimate those values. Readiness is more about a lack of negative values than a demonstration of peaking.
Response: You can track the effects of work or strain on the body using several systems listed in this guide, but typically the more medical the device, the more likely it’s used to track injury or pathology.
Performance: Muscle performance tests, such as muscle strength, are direct or isolated effort tests. The limitation of muscle performance tests is that they are usually poor predictors of performance, but do have value for assessing risk.
Return to play (R2P) incorporates all of the spectrum, as it’s the final step before full participation when the core rehabilitation is over. Some R2P programs are very mild, meaning they minimize the loss of practice and competition participation and involve very little rehabilitation, but even those programs incorporate monitoring of the injury site and involved risk areas.
The Medical and Performance Relationship Explained
Injury can happen with any level of athlete, but a pattern has emerged with athletes who suddenly decrease performance having a higher rate of injury. As fatigue, poor training preparation, and overload increase, so does the risk of injury and the likelihood of poor performance. The pattern of poor performance and injury works both ways, as an injury can obviously decrease performance just as much as poor training can increase the risk of injury. An athlete who is constantly rehabbing will not be properly prepared to succeed without a full training period. Athletes who continuously struggle performance-wise could increase their risk of injury.

Simply put, the goal of all of the systems is to create a “sweet spot” in both workload in training and the recovery process. While it’s hard to know what a true optimal load is, it is safe to say that a point of diminishing returns exists when work rates exceed thresholds that athletes can recover from. Conversely, if workloads are not sufficient, specific and necessary adaptations to the body will not occur and risk of injury or performance incompetence will surface.
Athletes who continuously struggle with performance could increase their risk of injury. Share on XMuscle and joint function monitoring presents a very unique and valuable opportunity for teams, as the data is important and relevant to both medical and performance roles. Countless high-performance presenters have complained about or praised their organization for having “no silos” with staff, and the monitoring of muscle and joint status is the perfect way to connect both roles. The intersection between injury and performance is a grey area at best, but both roles can benefit from collaboration using instrumentation.
The Pioneering Systems in Muscle and Joint Function
Listed are the leading systems and promising systems that you should consider when adopting monitoring systems. Each system, except for the sonography machines, has unique metrics that represent specialized data on muscle, tendon, and joint systems. Some systems require extensive training and a medical license, while a coach with no training at all—just experience in following a protocol—can use others.
MuscleSound: This Colorado company’s software is a value-added feature to sonography, focusing on estimations of glycogen content and attempting to manage fatigue. They also provide very useful estimates of body composition with their system, as it’s similar to DEXA and other measurements of body fat and muscle. The company has focused more and more on markets beyond sports teams, and offers their system to researchers and those involved with fitness and health.
SuperSonic Imagine: Elastography is very similar to sonography, and SuperSonic’s imaging is a part of the elastography market. The company focuses on an array of health and disease areas beyond sports medicine, but you can use their system for real-time tracking of any tissue. The Washington-based company is an international provider to hospitals and they have recently started doing research on sports medicine. Their system is a major investment, requiring serious training and skills to use and interpret the imaging.
Terason, GE, SonoSite: Conventional sonography is considered medical imaging, but due to the safety benefits of the equipment, tracking tissue is possible daily if time is not a burden. Unfortunately, time is a burden with most teams and even researchers struggle to collect data regularly because of its time and interpretation requirements. Some very brilliant therapists use sonography to diagnose injuries, but most of the talented medical professionals also use it to track rehab progress beyond reported symptoms or exercise milestones. Additionally, due to the fact most of the companies provide a portable option, training camps and other off-site locations can be tracked as well. Fascicle length of muscle groups is currently a hot topic in research, and some progressive medical experts are doing this internally with their athletes.
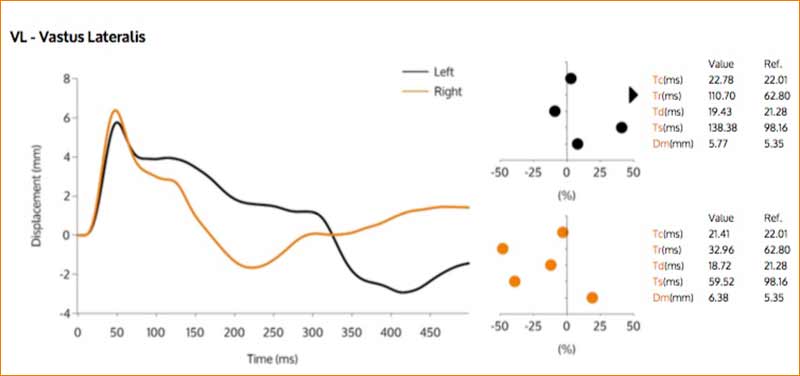
TMG-BMC: Tensiomyography is one of the strongest and most effective ways to evaluate skeletal tissue non-invasively and without imaging. The system uses electrical muscle stimulation to create a strong, involuntary contraction, and then extracts the contraction properties with a tensiometer, a gauge that can measure with precise sensitivity. TMG provides research-grade data rapidly and accurately, and the benefit is that anyone with training—regardless of role—can assess athletes. TMG is one of the most useful ways to track at-risk superficial muscle, such as adductors, hamstrings, calves, and groin muscles. In addition to muscle readiness and response to training, the system can estimate fiber composition of individual muscle groups. TMG has helped shape elite sport for decades, and their clients range from gold medal athletes to champion league soccer winners.
Vald Performance: Handheld dynamometers are very clinical, but they are usually for the assessment of small muscle groups or evaluations of general populations. Vald Performance has two key products: a hamstring testing solution and a groin evaluation device. The Nordbord, or hamstring test system, requires a Nordic hamstring exercise done on the equipment and relies on force transducers to estimate force from each angle. The data is then sent to a laptop and the test is scored and charted. Similar to hamstring evaluation, the Groin Bar evaluates the strength of the hip, but due to the complexity of the region, it’s only able to get abduction and adduction. Elite sport teams, both professional and college level, extensively use Vald.
Genourob: Genourob’s GNRB is the only arthrometer listed, as most of systems are muscle tissue tracking tools, but this solution from France is a ligament laxity testing device. The GNRB evaluates motion of the anterior cruciate ligament of the knee, and has a high degree of accuracy in detecting small tears. Clinicians in orthopedics have numerous manual tests to detect injury, but medical imaging usually defines the degree of injury, not physical testing by equipment. This device is intriguing because laxity may increase over time, thus increasing the risk of an acute injury. So far, such a theory is unproven, but on paper the concept is very similar to the cumulative injury theory we see with other models.
ThermoHuman and FLIR: Medical thermography uses IR cameras to track surface skin temperature, and those patterns do indeed have a relationship with muscle recruitment and work rates. Superficial heat is not a diagnostic tool or direct measure of fatigue, as skin temperature isn’t indicative of neuromuscular power. On the other hand, patterns over time in conjunction with other data sets do paint a very stark picture with risk to injury and the severity of chronic inflammation that could lead to more severe problems. ThermoHuman is an added-value software as a service option for teams and universities, and they objectively look at the body to establish a modified working baseline. Much of the innovation in sports thermography comes from equine sport, and the success of Spanish soccer has recently reignited its popularity.
Myoton: A small company in Estonia provides the last system, which estimates muscle tone and stiffness. The solution is more cost-effective, and is especially useful for lean athletes as a fat layer does make readings difficult. Simply put, the system is a digital palpation tool, and many therapists use it to see changes in their therapy. Due to the simplicity of the system and speed of the evaluation, many manual therapy practitioners use Myoton to decrease hypertonic tissue and to see trends in injury. Researchers working with stroke victims and those with Parkinson’s also use the system. The Myoton solution is a handheld device, and its data easily exports into an Excel file.

Some systems are more medical than others, and some fall so close to the diagnosis side that they are only on this list to demonstrate the fine line between monitoring and injury confirmation evaluation. The most important feature of all the systems is enough satisfactory evidence to show that they are valid. Some systems are very limited and they are not appropriate for all athletes, but all of the systems do have a role in elite sport.
Before Adopting Soft Tissue Monitoring Technology
Education and application are absolute requirements before adopting this technology. Unfortunately, it is common to invest before knowing how to use a system properly, as the pressure to solve injury problems usually leads to panic sales or similar. Education is not the same as training, as learning how to use the equipment is far different than learning how to apply the measurement approach.
Injuries are not just a medical problem—they are a team responsibility. Share on XInjuries are not just a medical problem—they are a team responsibility, starting with management and trickling down to the coaching and support staff. Athletes are also part of the equation, and they need to be involved and cooperative during testing for any solution to work. It is all too common for teams to invest in multiple systems, as no one system can solve every problem, but starting with one and expanding year to year is likely the best path to success in the long run.
Since you’re here…
…we have a small favor to ask. More people are reading SimpliFaster than ever, and each week we bring you compelling content from coaches, sport scientists, and physiotherapists who are devoted to building better athletes. Please take a moment to share the articles on social media, engage the authors with questions and comments below, and link to articles when appropriate if you have a blog or participate on forums of related topics. — SF
[mashshare]





1 comment
Dr. Samuel Pegram
Muscle monitoring is best possible only after you make a choice after MRI scanning of the knee. This will give you a significant advantage and you will feel a lot better. For the players involved in running sports such as football, this would become a significant advantage that the performance of knee will be monitored.