[mashshare]
In our concussion return to play (RTP) protocol, we have reduced premature returns to full activity by capturing and evaluating athlete exertion levels. Our protocol acts as a safety net to catch athletes at Central Michigan University (CMU) who are unable to meet exertional goals or whose symptoms return during the process, preventing them from moving to the next step of the protocol.
The NCAA Injury Surveillance Program showed 1485 concussions sustained by 1410 student-athletes from the 2011-2012 through 2014-2015 academic years. The average annual risk for football athletes is 5.42% while the average number of concussions per football team in a season is 5.63. Of all football teams, 80.6% reported a concussion per football season.
Over the past few years, a variety of organizations have invested a great amount of resources into research to better diagnose, understand, and treat the condition as well as to investigate the long-term effects of concussion and trauma to the brain.
Understanding Concussions: A Priority in Sports
Upon my arrival as Associate Head Athletic Trainer and Head Football Athletic Trainer at CMU, one of my first tasks was to review the Concussion Management Plan. With Dr. Matthew Jackson, CMU’s Medical Director, we identified items we needed to update to the standard medical consensus for concussion management.
At the root of our concern was that concussions were diagnosed primarily with subjective information in the past. This included the patient’s description of their symptoms, mechanism, history, and how they felt. Also, some objective testing measures (SCAT3 and BESS) still involved subjectivity as clinicians complete the ratings. This causes variability and, therefore, creates a minimal delectable change value that we have to take into account.
Dr. Matthew Jackson, Medical Director and Head Team Physician at CMU, states:
“The care of concussions has evolved significantly over the last five years. The heart of the diagnosis process, however, is still dependent on an honest report of the student-athlete symptoms, which is subjective. The name of the game to improve concussion diagnosis and return is the implementation of objectivity. Objective quantitative data is data that can be measured numerically and measured precisely, rather than through interpretation.
With concussions, one of the first objective assessments is the ImPACT neurocognitive testing, using a battery of tests compiling values for memory composite (verbal and visual), visual motor speed composite, reaction time composite, and impulse control composite. The test is also examined on a global cognitive efficiency index, which measures the interaction between accuracy (percentage correct) and speed (reaction time) in seconds on the Symbol Match Test.”
Many assessments and tools have since been developed that eliminate subjectivity and allow objectively diagnosed concussions. “Our department reanalyzed areas of the concussion diagnostic and return process to find areas that were amenable to obtaining objective measurements, the first one identified was balance or postural sway,” Dr. Jackson explains.
At CMU, we have taken steps to objectify our assessment of balance–or postural sway–given that it’s a primary symptom or disability used to diagnose a concussion. We’ve eliminated the BESS test which has some subjectivity with large minimal detectable changes for either inter-rater reliability or intra-rater reliability.
We started using Biodex’s BioSway. The system has a force plate that measures postural sway, or movement of the center of mass from the center point. The force plate and sensors measure this data and provide an output that allows us to have objective data to determine disablement of balance or postural sway, due to concussion, in relation to a baseline value.
John Bonamego, CMU Head Football Coach, states:
“Since my arrival as the head football coach at Central Michigan University, our Sports Medicine Department has undergone consistent changes and improvements. One primary focus of improvement has been the Concussion Management Plan, specifically the return to play process for the student-athletes.
This process is now thorough and extensive to ensure player safety, which is our number one priority as coaches who are responsible for the health and well-being of the student-athletes. When students are recruited to become football players at Central Michigan University, we express to their parents and guardians that their physical and mental health is of the utmost importance, and with this plan and process for the care and progressive return to play, we stand behind our promise.”
Objectivity regarding a patient’s exertional progression has been slower to integrate into the concussion RTP protocols. “One area that I believe is one of the most critical parts of the RTP process is where cardiovascular exertion is meant to identify lingering concussion symptoms that are present before advancing through the protocol and ultimately cleared for sport participation,” Dr. Jackson states.
Two Standard Return to Play Protocols for Concussions
- One of the first recommendations for RTP protocols came from the Consensus Statement on Concussion in Sport: The 4th International Conference on Concussion in Sport held in Zurich in 2012.
- Day 1. Rest: 24 hours asymptomatic
- Day 2. Light aerobic exercise: <70% MHR
- Day 3. Sport-specific exercises: running drills, skating drills
- Day 4: Non-contact training drills: complex drills, passing drills
Day 5: Full contact practice: after clearance - Day 6: Return to play
- The NFL Head, Neck, and Spine Committee developed this RTP protocol for all the teams under their organization.
- Day 1. Rest and recovery: return to symptom and neurological baseline
- Day 2. Light aerobic exercise: stationary bike, treadmill
- Day 3. Continued aerobic exercise and introduction of strength training: increased cardiovascular exercises and may mimic sport activities, introduce strength training
- Day 4. Football-specific activities: non-contact football activities
- Day 5. Full football activity/clearance: after clearance
It has been assumed that an athlete, on day 2, was less than 70% based on verbal instructions to “not break a sweat, pedal at 70%, etc.” On day 3, it has been assumed that causing the athlete to perform a more difficult cardiovascular exercise (i.e.- stair step,elliptical, swim-ex, etc.) would exceed greater than 70% of the max heart rate with similar verbal instructions.
Exertional Testing for Return to Play After a Concussion
To determine an athlete’s true exertion level during the return to play process, we decided to integrate objective measures, if possible. Our first idea was to integrate HR monitors with the athletes. We realized that heart rate would fluctuate so we wouldn’t have a reference output or ability to determine a constant threshold, but it would be a step toward greater objectivity when considering exertion levels for return to play.
Why is it so important to test exertion during the return to play process? Through research efforts, the medical community learned that stressing the human body with exercise stresses the physiologic systems (cardiovascular system, neurological system, respiratory system, muscular system). When a concussion has not resolved, an athlete’s exertional stress to these systems can cause the symptoms to return. There lies the importance of stressing the system to a level that instills confidence that the concussion has resolved enough to move to the next step of the return to play process.
We fear that the lack of objective data to determine exertional levels to the system creates a great limitation where athletes can “cheat the system” and advance to the next step in the protocol when their body and brain are not yet prepared.
“Once symptoms from the concussion have resolved, the student-athlete often wants to get back to sport as fast as possible and sets up the possibility for underreporting symptoms during the exertional component of the return to play protocol,” Dr. Jackson describes.
Underreporting could ultimately cause an athlete to return to competition too early, precipitating the potential for relapse of symptoms, repeat trauma, or a post-concussive syndrome. With objective exertional measurements, we hoped to eliminate the risk of repeat traumas to the brain when it has not recovered.
Objective exertional data can decrease the risk of repeat trauma to an unrecovered brain with an unresolved concussion. Share on XThe HiTrainer gave us the best opportunity to accomplish our goals of integrating objective measures. I was exposed to the HiTrainer when I arrived at CMU through my initial collaboration with Jason Novak, Director of Strength and Conditioning at CMU. Novak brought the equipment to CMU upon his arrival as the Director of Strength and Conditioning and used the equipment in a variety of ways to develop athlete performance.
Novak states, “The implementation of the HiTrainer into our strength and conditioning program has been one of the best additions we have made in my three seasons here at CMU. It allows us to target specific areas of need on an individual basis. The HiTrainer provides us with the ability to train our athletes at various intensities with quantifiable outputs such as distance, speed thresholds, power outputs, and right/left asymmetry. We no longer have to go by ‘feel’ or just athlete feedback based on of rates of perceived exertion (RPE). We can accurately measure effort, output, and improvement including comparisons of pre- and post-injury.”
Our medical staff was interested initially in the power outputs and right to left asymmetry for uses ranging from post-surgical rehabilitation to neuromuscular feedback processes. “We are now capable of integrating sport-specific conditioning protocols for individual athletes in a controlled environment with specific goals and thresholds that are appropriate for each athlete and their current state of conditioning,” Novak explains.
It’s the threshold training that sparked our use of the system for objective measurement of exertion for concussion return to play. The development of the HiTrainer Concussion RTP step came next.
CMU Sports Medicine Department Concussion Return to Play Protocol
- Day 1. Asymptomatic for 24 hours: rest
- Day 2. Light aerobic exercise: <70% max HR on stationary bike for 30 minutes
- Day 3. Advanced aerobic exercise: between 70-95% on HiTrainer RTP protocol for 30 minutes
- Day 4. Non-contact sport practice and introduction of strength training activities: sport-specific drills and strength training session
- Day 5. Full contact practice after baseline diagnostics: returned to baseline on all assessments, after clearance
- Day 6. Return to competition/games
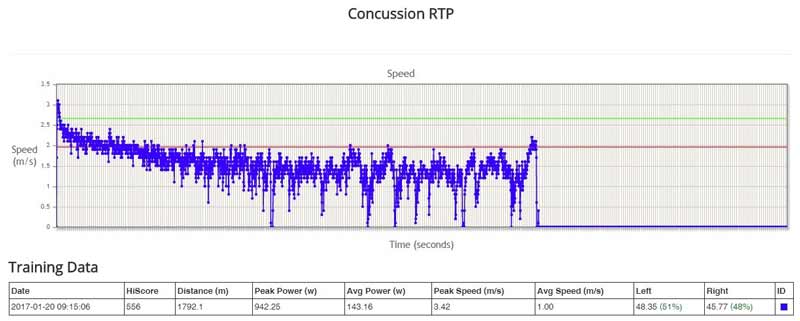
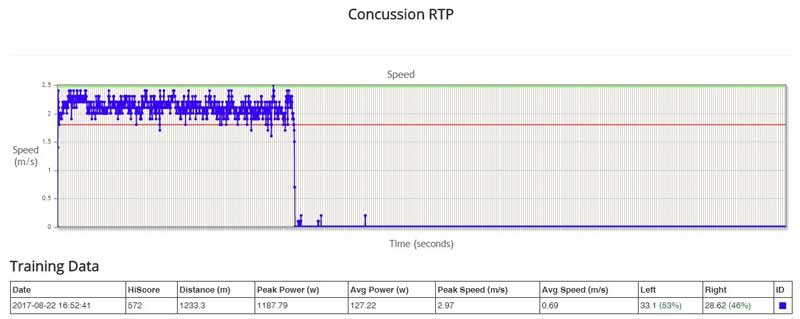
By using the HiTrainer Pro’s Threshold Training options, we’ve set an exertional standard and have some objective output to ensure that our athletes hit the standard. We accomplish this by having an athlete complete a one-minute max effort walking rep to determine their average speed over the minute timed. We take 70% and 95% of the average speed to determine our upper level threshold and lower level threshold.
These thresholds are displayed on a tablet, which the athlete uses to stay within the thresholds while completing a 30-minute walk on the HiTrainer. Athletes must spend the majority of time within the threshold, without the return of symptoms, to advance to the next day of the RTP protocol.
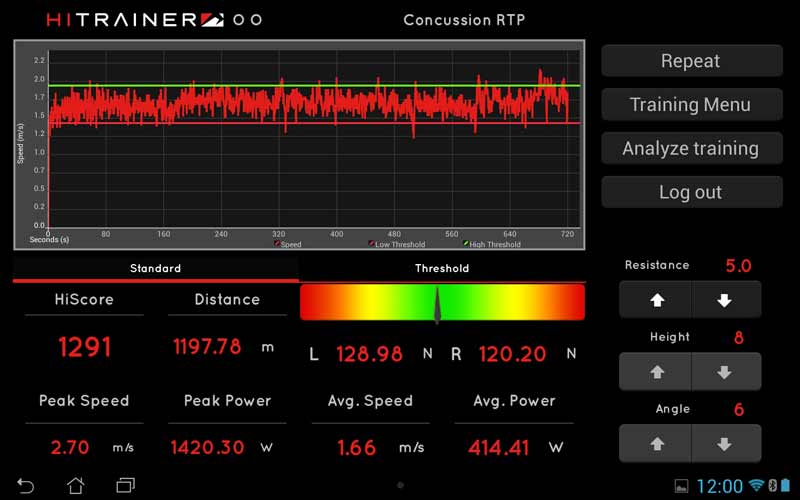
This HiTrainer Concussion RTP protocol constitutes Day 3 of our concussion return to play protocol. We print the report from the HiTrainer RTP and place it in our medical records, aiding in documentation with objective data measures. We believe the use of the HiTrainer lessens the “gap” or “jump” seen from Day 2 to Day 4. Since Day 2 introduces cardiovascular stress to the system and Day 4 is functional activity including stress to all systems, Day 3 has to marry these and meet in the middle to have a truly successful increase in exertional demands placed on the human body.
The HiTrainer accomplishes this better than equipment we’ve used in the past due to the ability to set exertional goals, objectively assess the ability to reach or complete these goals, and create a visual stimulus by having the athlete focus on the tablet displaying the thresholds they must stay within. This causes “now” stress on the neurocognitive system to react and maintain the rest of the body’s systems to reach the exertional goal.
Dr. Jackson admits, “by having a very objective and quantifiable test that more closely simulates sports activity, we can standardize this aspect of the return to play process. The HiTrainer allowed for a very consistent and increase in difficulty for exertional testing that may expose a lingering concussion injury whose symptoms have resolved.”
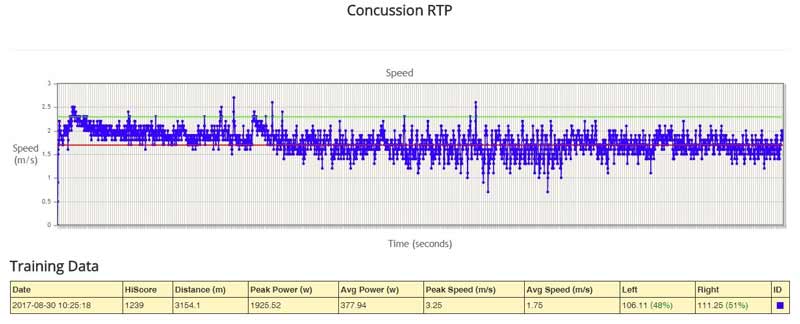
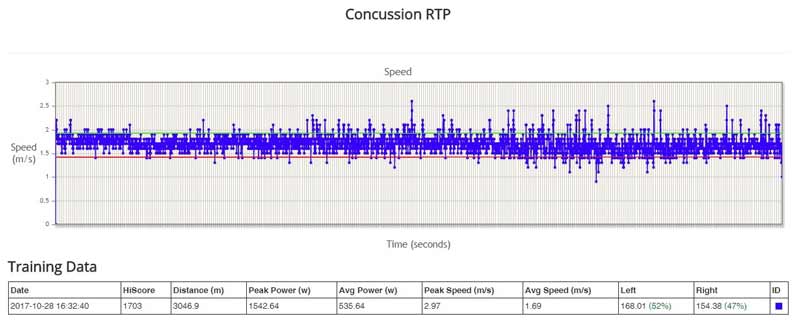
We’ve used the HiTrainer for over a year, and it has decreased premature returns to full activity; it performs as an objective measurement tool to help us meet exertional expectations and goals in a concussion RTP protocol. “Furthermore the student-athlete consciously or unconsciously is not able to reduce effort in order to avoid symptom onset and at the end of the day allows us to be very confident when the athlete completes the exertional testing using the HiTrainer,” Dr. Jackson explains.
Using athlete exertion levels in concussion protocols reduced premature returns to full activity. Share on XThe HiTrainer Concussion RTP is a safety net, catching athletes who are unable to meet the exertional goals or who have the return of symptoms during the process, eliminating their opportunity to move to the next day of the RTP protocol. Using the HiTrainer as part of our Concussion Management Plan in the RTP protocol, we’ve seen fewer relapses of concussion symptoms later in the RTP protocol or after full clearance for competition.
“The use of the HiTrainer in the concussion return to play also instills confidence in the individual student-athlete that we are doing everything possible to make sure the concussion has truly resolved and that their body is ready to take on the load that occurs in participating in college athletics,” Dr. Jackson states.
From October of 2016 to October of 2017, 28 student-athletes completed the HiTrainer protocol in their return to play process from a concussion at CMU. Of the 28, only three student-athletes had repeat concussions or symptom onset.
- Athlete 1, a collegiate football player, was nine months between concussion diagnoses. Both concussions occurred during in-season contact football–the 2016 and 2017 seasons.
- Athlete 2, also a football player, was only one month between concussion diagnoses in the 2017 season; the medical staff viewed these as two independent concussion events.
- Athlete 3 experienced a return of concussion symptoms fewer than two days after returning from a medically-cleared resolved concussion based on completion of the RTP protocol and return to baseline on all assessments.
It came to light that Athlete 3 was not truthful with his subjective reporting and placed himself at risk; his brain had improved enough to pass the RTP protocol and concussion assessments but not enough to return to participation. This goes to show that, even with technologies to diagnose concussions and stop an athlete with a concussion from returning too early, we still have to rely on athletes reporting their symptoms. Head Coach John Bonamego explains:
“Our Sports Medicine Department has done a great job with integrating technologies to improve the diagnostic and return process of concussion, specifically the step using the HiTrainer to make sure athletes are reaching exertional goals to test their bodies. This gives us great confidence as coaches that when someone returns from a concussion and is cleared to participate by the Sports Medicine Department that they have truly resolved from the concussion and are prepared and safe to take on the stress placed on the body by the game of football.
We here at Central Michigan University do not want a student-athlete back on the field if they are not physically and mentally prepared to return to sport. I believe this process also gives great confidence to the student-athletes who suffer a concussion to definitively know they are ready and capable of return to sport upon the completion of our return to play process.”
Return to Play with Evidence
We’ve made a strong step forward using the HiTrainer in the RTP protocol. However, we have more to do, and it’s exciting that HiTrainer, as a company, shares these beliefs. It is working on developing the system to improve the objectivity of the exertional data, to be 100% individualized to the athlete, and to accommodate factors like fatigue at the end of the protocol.
This constant effort to think outside the box and promote continued advancement in concussion diagnostics and return to play is not only appropriate but also necessary. The company is committed to promoting athletes’ safe return whether from concussions or orthopedic injuries. The HiTrainer is extremely multifaceted and can be used as a performance-enhancing tool as well as a rehabilitation tool.
At CMU, the HiTrainer is a staple in not only the Strength and Conditioning Department but also the Sports Medicine Department. We are fortunate to be one of the few colleges and universities at this time to have access to the equipment and to have entered a partnership for advancement that will aid the health, safety, well-being, and performance of all CMU student-athletes.
Since you’re here…
…we have a small favor to ask. More people are reading SimpliFaster than ever, and each week we bring you compelling content from coaches, sport scientists, and physiotherapists who are devoted to building better athletes. Please take a moment to share the articles on social media, engage the authors with questions and comments below, and link to articles when appropriate if you have a blog or participate on forums of related topics. — SF
[mashshare]




