
Jason Avedesian is a post-doctoral researcher at the Emory Sports Performance and Research Center. His research focuses on how sports-related concussions and neurocognition contribute to lower-extremity injuries in athletes. Jason has spent time at all levels of sport (adolescent, collegiate, professional) and enjoys working with athletes to achieve their performance goals.
Freelap USA: ACL injury is running rampant in youth sports today. What are the key mechanisms to this sport injury?
Jason Avedesian: I’m going to take this question and provide a little bit of historical context into how ACL injuries have been viewed over the last two decades.
Early 2000s ACL research provided us with some of the first data on the biomechanical mechanisms associated with high risk for ACL injury. When looking at ACL injury purely from this perspective, we can think of it as an injury due to tri-planar knee motion (sagittal + frontal + transverse planes). Specifically, ACL injuries predominantly occur during single leg jumping, cutting, or deceleration movements.
Injured athletes often (but not always) demonstrate a low knee flexion angle combined with excessive knee rotation and side-to-side knee motion. With contributions from the hip and ankle joints, this knee pattern is commonly referred to as dynamic knee valgus. While these biomechanical mechanisms were important to establish, they do not always provide a clear cause-and-effect relationship, at least from a laboratory-based assessment.1 The next question became, how do these biomechanical risk factors emerge while an athlete is in competition?
In the early-to-mid 2010s, larger-scale video analyses were conducted to determine situational patterns associated with actual ACL injury events. While most injuries were non-contact, these video-based studies revealed that athletes were often sustaining ACL injuries during an attacking scenario when near opposition.2,3 Often, the athlete’s visual attention appeared to be focused everywhere except their own movements. This has led me and other researchers to begin investigating how visual performance and neurocognition may contribute to ACL injury.
Inefficient sensorimotor abilities (anticipating and responding to environmental cues on the field) also need to be considered a mechanism for ACL injury, says @JasonAvedesian. Share on XWhen athletes perform tasks that stress attention and decision-making, they often demonstrate biomechanical patterns that are associated with greater risk for ACL injury.4 While much more research and data are certainly required, we are beginning to think that inefficient sensorimotor abilities (anticipating and responding to environmental cues on the field) also need to be considered a mechanism for ACL injury.
Freelap USA: What global components are most often missed in training programs that can have a large impact on ACL risk?
Jason Avedesian: When strictly looking at ACL injury risk, I like to think of training programs in four interrelated parts: the warm-up, strength training, plyometrics, and agility. Most programs do a pretty good job with strength training. To me, the key to reducing ACL injury risk is giving as much time and thought to the other three components.
Let’s start with the warm-up. I would argue it’s the most important part of training. Sports-specific warm-ups have been demonstrated to significantly reduce the risk of lower body injuries numerous times, including the ACL.5–7 Think of the warm-up as the way to “wake-up” the neuromuscular system.
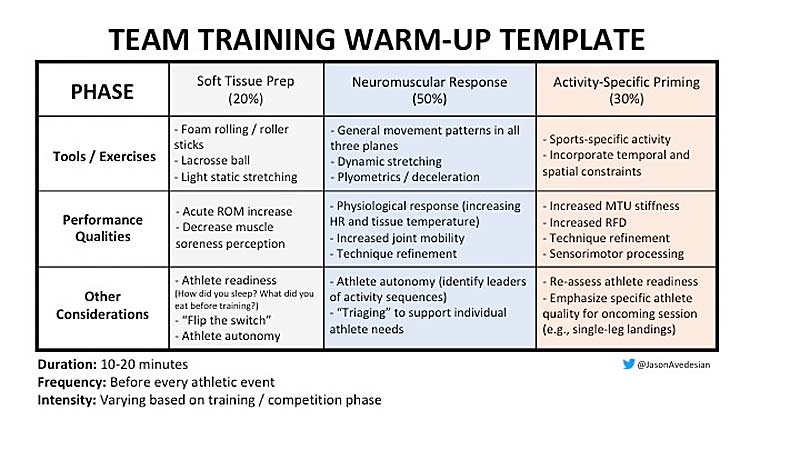
A well-designed warm-up will elevate physiological responses such as heart rate, tissue temperature, tendon stiffness, and post-activation muscular performance enhancements.8 I like to break down the warm-up into three phases: soft-tissue prep, neuromuscular response, and activity-specific priming. The template below provides a general warm-up outline that can be adopted to suit your athletes’ needs.
Plyometric training is another component that certainly needs your attention. You need to consider this: most ACL injuries occur during single-leg deceleration maneuvers. Whether it be a jump cut or jump landing, athletes typically get injured when most of their body weight is on a single leg. Therefore, your plyometric training should reflect these demands. Programming plyometrics will certainly depend on athlete skill level, but here are my general recommendations:
- Emphasize quality over quantity. Plyometrics should be low-volume, high-intensity training. I generally program with low repetitions and moderate-to-long recovery periods.
- Progress plyometrics from double leg to single leg. It may not look pretty at first, since in my experience, athletes initially struggle to maintain stability during single-leg plyometrics. However, consistency with single-leg training will be very beneficial in the long term.
- Include external objects and/or teammates. Especially when it comes to ACL injury, we’re always looking for ways to be more “sports specific.” A few ways to do so could include athletes passing and catching objects or having to make anticipatory/reactionary responses to teammates during plyometric training.
Lastly, we can leverage agility training to reduce the risk of ACL injury. I’ve found there is some confusion about the differences between agility and change of direction (COD).
While both COD and agility training certainly have merit within a training model, it’s important to distinguish between the two. An athlete performs a COD maneuver when movement is pre-planned, whereas an agility maneuver is performed when movement is in response to a stimulus.9
COD training is inherently stable (i.e., athletes know exactly where to go and when to change direction), whereas agility situations present an athlete with conditions that help train anticipation, reaction time, and decision-making. Agility training can come in many forms, such as small-sided games, 1 vs. 1 drills, and tag-like games. You can certainly get very creative with designing agility training, but the important point is that you should ultimately strive to put athletes in practice conditions where they must perform sports-specific movements that are not pre-planned!
Freelap USA: It is commonly understood that females have a higher risk of ACL injury. Why is that? How do we combat that risk?
Jason Avedesian: The numbers vary from study to study, but generally female athletes are at a 2-4x greater risk for ACL injury.10 Initially, it was believed that elevated ACL injury rates in females were due to non-modifiable, intrinsic risk factors (anatomical structure, hormone differences).11 As more evidence became available, the research often demonstrated that females performed sports tasks (e.g., jump landings and jump cuts) with biomechanical patterns associated with greater risk for ACL injury (i.e., greater knee valgus, decreased hamstring activity).
While these intrinsic risk factors certainly contribute to ACL injury in the female athlete, we need to also consider extrinsic risk factors such as psychosocial and cultural influences.12 Are female athletes being encouraged to train like their male counterparts? Do females have access to similar resources? Although the perception of training for female athletes is much improved compared to previous decades, there are still certain myths that linger: strength training is dangerous (it’s not), light weights should be used to “tone muscle” (not accurate), and females will become “big and bulky” (strength training 2-3x per/week will certainly not turn a female athlete into a bodybuilder).
A large amount of data indicates that neuromuscular training (strength + plyometrics + stability) 2-3x per week for ~30 minutes can significantly reduce the risk of ACL injury in female athletes. Share on XThe first barrier we need to overcome is getting female athletes (along with parents and coaches) to “buy in” to training for their sport. There is a large amount of data indicating that neuromuscular training (strength + plyometrics + stability) 2-3x per week for ~30 minutes can significantly reduce the risk of ACL injury in the female athlete.13 Read that sentence one more time. And then again.
While this seems very, very simple, this barrier is the hardest one to cross in this athlete population, especially at the adolescent level. My recommendation if you are looking to start a training program with female athletes: reach out to a strength and conditioning and/or sports medicine professional to get the best information for how to effectively train for the purposes of ACL injury risk reduction.
Freelap USA: Every surgeon’s return to play protocols for ACL repair can be slightly different. In your experience, what can we improve to reduce the likelihood of reinjury?
Jason Avedesian: ACL reinjury rates are considerably high, especially in the adolescent population. In the unfortunate situation where an athlete does sustain an ACL injury, I think the best way to reduce the likelihood of reinjury is through a multidisciplinary approach. As an ACL researcher and S&C coach, I want to be in communication with all the vested parties, including the parents/family, surgeon, physical therapist, and sport coaches. This concept can be thought of as an athlete-centered approach. For example, the data and information I collect from the sports science and S&C side can help facilitate targeted practices for the physical therapist (and vice versa), which can then help the athlete, surgeon, coaches, and parents better understand the time course of recovery and any underlying risk factors that we can mitigate early in the rehabilitation process.
Unfortunately, this type of approach to injury rehabilitation (and ACL injury risk reduction in general) is not all that common for several reasons (feasibility, silo effect in the various disciplines, etc.), but there are solutions available. For starters, sports scientists need to continue to be active in terms of disseminating knowledge through mediums other than peer-reviewed papers. To be frank, most practitioners and coaches do not have the bandwidth to dive through publications with complex statistics and little real-world validity. They just want to know what works and what doesn’t.
Most practitioners and coaches do not have the bandwidth to dive through publications with complex statistics and little real-world validity. They just want to know what works and what doesn’t. Share on XAlong these same lines, the ability to quantify and visualize information easily can have an immense impact. Cost-effective wearables and software offer good solutions for these purposes, but again it comes back to having a multidisciplinary team to decipher what is effective for the athlete. Breaking down silos and continuing to pump out good, easily accessible information is ultimately one of our best weapons for combating the ACL injury problem.
Freelap USA: According to your research, ACL injury has a high neurological component. How do we include those types of stimuli into training?
Jason Avedesian: Back in my master’s, I focused solely on the biomechanical aspects of ACL injury (see question 1). My Ph.D. research (the relationship between sports-related concussion and lower-extremity injury in adolescent and college athletes) made me start to ponder, was biomechanics really the answer to our ACL injury problem? Or was there something happening even further up the chain that we could target for injury risk reduction? Ultimately, this has led me to exploring the central driver of neuromuscular control…the brain!
When I think of how the brain plays a role in ACL injury, five macro-level variables come to mind:
- Visual Attention – Stimulus arriving at the eyes and being relayed to higher processing brain areas responsible for information processing, working memory, and pattern recognition.
- Reaction Time and Processing Speed – This is part of a concept known as visuo-motor integration, in which a neuromuscular response is completed based upon how the visual system recognizes and processes a stimulus.
- Impulse Control – The ability to identify relevant or irrelevant stimulus and act or resist upon this recognition.
- Working Memory – Short-term, limited capacity information processing that helps guide anticipation and decision-making.
- Stress and Anxiety – This is very important, as feelings of emotional tension can influence the other four variables.
Videos 1-3. A progression from Corey Peterson moving from a closed change of direction drill to agility training with dynamic, reactive elements.
At this point, the research has told us that athletes with slower reaction times, worse working memory, and higher levels of stress/anxiety are at greater risk for lower body and ACL injuries.14–19 Luckily, there are ways that we can monitor and train these components with our athletes. For stress and anxiety, the use of questionnaires can be a very cost-effective and feasible way to monitor and intervene during highly stressful periods (e.g., final exam weeks, playoffs). The other neurocognitive variables can be targeted and trained through more technological-based equipment (sensory boards, stroboscopic eyewear, etc.) and agility training.
When thinking of ways to train the neurocognitive system as it relates to ACL injury risk reduction, I suggest starting at the eyes. About two-thirds of all sensory receptors in the body are located in the eyes, and 40% of the cerebral cortex is dedicated to vision.20 On the field, athletes navigate very complex environments in which visual information is constantly changing.
When thinking of ways to train the neurocognitive system as it relates to ACL injury risk reduction, I suggest starting at the eyes, says @JasonAvedesian. Share on XThis all comes back to my point about the key difference between COD and agility. When athletes respond to visual stimuli in sport, they are performing agility-type maneuvers. Videos 1-3 are a great example of an agility video progression from Corey Peterson at the University of Minnesota, who is doing great work in terms of agility training with his athletes. Notice the progression in visual information processing. Like all things in training, you need to specify to your athletes and their needs. But thinking of how the neurocognitive system plays a role in ACL injury risk will ultimately start to get us heading in the right direction.
Since you’re here…
…we have a small favor to ask. More people are reading SimpliFaster than ever, and each week we bring you compelling content from coaches, sport scientists, and physiotherapists who are devoted to building better athletes. Please take a moment to share the articles on social media, engage the authors with questions and comments below, and link to articles when appropriate if you have a blog or participate on forums of related topics. — SF
References
1. Cronström A, Creaby MW, and Ageberg E. “Do knee abduction kinematics and kinetics predict future anterior cruciate ligament injury risk? A systematic review and meta-analysis of prospective studies.” BMC Musculoskeletal Disorders. 2020;21:563.
2. Carlson VR, Sheehan FT, and Boden BP. “Video Analysis of Anterior Cruciate Ligament (ACL) Injuries: A Systematic Review.” JB&JS Review. 2016;4:10.2106/JBJS.RVW.15.00116.
3. Della Villa F, Buckthorpe M, Grassi A, et al. “Systematic video analysis of ACL injuries in professional male football (soccer): injury mechanisms, situational patterns and biomechanics study on 134 consecutive cases.” British Journal of Sports Medicine. 2020;54:1423-1432.
4. Hughes G and Dai B. “The influence of decision making and divided attention on lower limb biomechanics associated with anterior cruciate ligament injury: a narrative review.” Sports Biomechanics. 2021;1-16.
5. Owoeye OBA, Akinbo SRA, Tella BA, and Olawale OA. “Efficacy of the FIFA 11+ Warm-Up Programme in Male Youth Football: A Cluster Randomised Controlled Trial.” Journal of Sports Science and Medicine. 2014;13:321-328.
6. Silvers-Granelli H, Mandelbaum B, Adeniji O, et al. “Efficacy of the FIFA 11+ Injury Prevention Program in the Collegiate Male Soccer Player.” American Journal of Sports Medicine. 2015;43:2628-2637.
7. Herman K, Barton C, Malliaras P, and Morrissey D. “The effectiveness of neuromuscular warm-up strategies, that require no additional equipment, for preventing lower limb injuries during sports participation: a systematic review.” BMC Medicine. 2021;10:75.
8. Blazevich AJ and Babault N. “Post-activation Potentiation Versus Post-activation Performance Enhancement in Humans: Historical Perspective, Underlying Mechanisms, and Current Issues.” Frontiers in Physiology. 2019;10:1359.
9. Sheppard JM and Young WB. “Agility literature review: classifications, training and testing.” Journal of Sports Sciences. 2006;24:919-932.
10. “The female ACL: Why is it more prone to injury?” Journal of Orthopaedics. 2016;13:A1-A4.
11. Hewett TE, Myer GD, and Ford KR. “Anterior cruciate ligament injuries in female athletes: Part 1, mechanisms and risk factors.” American Journal of Sports Medicine. 2006;32:299-311.
12. Parsons JL, Coen SE, and Bekker S. “Anterior cruciate ligament injury: towards a gendered environmental approach.”British Journal of Sports Medicine. 2021;55:984-990.
13. Sugimoto D, Myer GD, Barber Foss KD, Pepin MJ, Micheli LJ, and Hewett TE. “Critical components of neuromuscular training to reduce ACL injury risk in female athletes: meta-regression analysis.” British Journal of Sports Medicine. 2016;50:1259-1266.
14. Wilkerson GB. “Neurocognitive reaction time predicts lower extremity sprains and strains.” International Journal of Athletic Therapy and Training. 2012;17:4-9.


Really enjoyed this article thank you. If we are suggesting that working memory may be linked to lower limb injury, how does that relate to the huge number of athletes with dyslexia and processing speed and memory deficits? When completing baseline concussion cognitive tests I have watched athletes with dyslexia really struggle even without having had a concussion and wonder about how accurate the testing might be