In almost 10 years, my search for the ideal recipe for optimized recovery has had the scent of an epic…the quest for my Holy Grail, so to speak! I’ve tried crazy, futuristic technologies including floating tanks, hyperbaric chambers, lasers of all kinds, and gadgets worthy of James Bond. I’ve attended lectures from great doctors and famous scientists and started talking about biohacking with engineers straight out of Google’s “dream factory.” In this quest, I’ve also had to oust snake oil vendors and other new druids peddling magic potions and fancy powders.
Many times, I have found myself grappling with questionable practices so folkloric that one would almost excuse the quasi-total absence of their scientific basis. Perhaps you have experienced the same story? Or are you still outside, with your sleeves rolled up, determined to find this elusive recipe?
Good luck.
Each individual is different, and each athlete is a complex system in their own right. As Louie Simmons said, everything works, but not forever. Varying recovery techniques may be as important to keeping an athlete on their feet as varying workouts. Strength session and the troops are sent to take cold baths; endurance session and the same recovery modality is used again. Morning or evening, preseason or final week. Let’s stop for a bit. We can do better if we take the time to rethink how we prescribe recovery.
Cold Is Not the Answer
Since 1978, two things haven’t changed: the music of the Bee Gees continues to loop in discotheques and the RICE protocol (rest, ice, compression, elevation) continues to be systematically applied for the treatment of sports injuries. Ice is a standard treatment for injuries and muscle pain because it helps relieve pain caused by injured tissue. Pulling the cold baths and icing cards from the magic hat of recovery techniques to apply in all circumstances was once my favorite trick. It was forgivable a decade ago, but it is now clear that ice and complete rest delay healing rather than help it.
It is now clear that ice and complete rest delay healing rather than help it. Share on XA recent study observed athletes required to exercise so intensely that they developed severe muscle damage causing extensive muscle pain.1 Although the cooling delayed the swelling, it did not speed up healing of the muscle damage. Furthermore, no evidence was found that ice and compression accelerated healing compared to using compression alone.
When muscles and other tissues are damaged, whether it is the result of injury or intense training, inflammatory cells rush to injured tissue to start the healing process. These inflammatory cells, called macrophages, release a hormone that is particularly important in the recovery and reconstruction of damaged tissue: insulin-like growth factor (Insulin Growth Factor 1, or IGF-1). The use of ice to reduce swelling tends to delay healing by inhibiting the body from releasing IGF-1.
That people are less concerned with IGF-1 than with the feeling of pain and swelling when an injury is fresh is understandable, especially if the athlete cannot be recovered in a short period of time. But cold exposure as a systematic, post-workout recovery strategy is absurd—especially in the preseason, when the goal is to induce adaptations requiring a large amount of inflammation (such as building muscle mass). IGF-1 is a potent anabolic agent and plays a central role in muscle and metabolic adaptations to exercise. Spending long minutes in a cold bath right after a hypertrophy session is a bit like having a Diet Coke with your Big Mac and fries. It doesn’t help the matter.
Applying ice to damaged tissue (and again, intense muscle training leads to damage, not just collisions) causes blood vessels to constrict in exposed muscles. This effect is not simply present during the application of ice, the blood vessels do not open for many hours after treatment. Vasoconstriction in muscles damaged and fatigued by exercise is a dramatic outcome in an attempt to optimize recovery. Cytokines and other inflammatory agents no longer have access to the area that requires their action, and the nutrients ingested will not reach their destination, compromising muscle glycogen stores. Moreover, the lymphatic system is slowed down and metabolic waste accumulates locally. Overall, this decrease in blood flow is a hindrance to recovery.
Cold exposure as a systematic, post-workout recovery strategy is absurd—especially in the preseason, when the goal is to induce adaptations requiring a large amount of inflammation. Share on XCold baths and icing are big favorites for intra-games activities in tournament-style sports, such as Sevens rugby. Cooling can help reduce pain, but it interferes with an athlete’s strength, speed, endurance, and coordination. A medical journal presented 35 studies on the effects of cooling, and most reported a decrease in strength, speed, power, and agility immediately after cooling.2
So, is it worth the effort?
Adiponectin and Overtraining Syndrome
I am not sick of the cold, make no mistake! Cold has multiple positive effects on recovery.
An interesting aspect of winter numbness is that it stimulates the production of adiponectin. This hormone, synthesized in adipose tissue, is involved in the regulation of glucose. Adiponectin increases muscle uptake of glucose—without a parallel increase in insulin—which reduces blood sugar.
Adiponectin is also the most potent anti-inflammatory adipocytokine. It strongly suppresses the production of the pro-inflammatory cytokine TNF-F, and recent studies show that it induces the production of various anti-inflammatory cytokines such as IL-10. This hormone, capable of increasing insulin sensitivity and endowed with anti-inflammatory properties, is said to have a considerable antidepressant and anxiolytic effect. When you consider the following sequence…

…the potential impact of adiponectin becomes clear. The concept of overtraining is complex, and there is still no consensus on its definition. Perhaps this is a gross exaggeration or perhaps this is an avenue to explore, but in view of the effects of adiponectin, cold therapy offers itself as a possible solution for the victims of overtraining.
Cold Exposure and the Immune System
Engaging in a cooling activity is also a great way to fight bacterial infections, seasonal viruses, and other temporary illnesses. Exposure to cold causes an increase in the number and activity of natural killer cells, as well as interleukin-6 available in the bloodstream, which strengthens the integrity of the immune system.
The cold contributes to better immunity through an additional phenomenon, the expression of the target of rapamycin (mTOR). Exposure to cold inhibits mTORC1 and starts a process of autophagy, in which the body destroys some of its own cells. This mechanism eliminates damaged cells and thus strengthens the immune system. Cold therapy at the time of the first symptoms, although counterintuitive, can therefore help to fight more effectively against an infection or a virus such as the common cold.
The use of cold should be prescribed for specific conditions:
- Urgent weight loss.
- Overtraining.
- Fragile health or immune depression due to a particularly grueling period (multiple long trips, congested schedule, etc.).
On the other hand, when the development of physical qualities or daily post-session recovery is the objective, you should generally avoid this strategy. (I hope I haven’t…cooled you off on the practice completely.)
Heat Shock Proteins: Role in Recovery
Swap your fleece suit for a swimsuit, and let’s explore the effects of heat exposure. The Native Americans adopted the sweat lodge; Scandinavians swear by their saunas; the soothing bubbles of a Jacuzzi or the steaming fog of a steam room are attractive after a week of hard work…there are many good reasons for this. Fifty years of scientific studies confirm the effectiveness of regular exposure to a hot environment.
Fifty years of scientific studies confirm the effectiveness of regular exposure to a hot environment. Share on XThere are several mechanisms at work here, and a primary one is heat shock proteins (HSPs). For 98% of human history, our ancestors were regularly exposed to heat. It was only with the advent of the Industrial Revolution and the crutch-turned-innovations that followed that we stopped suffering from the heat, at least in “developed” countries. Unless you are a runner who exercises in the African dunes or a diehard CrossFitter voluntarily exposing themselves to a risk of rhabdomyolysis, it is a safe bet that your training sessions (in their majority) take place either in an environment where the temperature is controlled or at a time of day when the temperature is milder.
The result? Your HSPs have gone into sleep mode, and with them a powerful way to regulate your immunity and deal with internal and external stressors. HSPs protect cells against stress. Secreted during and after physical exercise, they have several functions. Some researchers believe that increasing levels of peripheral HSP70 molecules participate in the perception of fatigue.
HSP70 plays a role in muscle repair by restoring the recruitment of muscle cells involved in the inflammatory response. Several studies report an association between muscle strength output and HSP70 levels, and the main function of HSPs at the muscle level is to support regeneration processes. Exposure to heat stimulates the same adaptations and can be used to mimic the regenerative effects of physical exercise at a lower energetic, mechanical, and psychological cost.
Post-Training Heat Exposure Increases Physiological Adaptations
More interestingly, heat exposure and exercise can be combined for even more benefits. The production of HSP results in a type of preconditioning of cells. With this preconditioning, subsequent stressors do not have the same impact as the initial event. Therefore, preconditioning or priming (thermal shock priming) can be used to “train” the internal environment. Exercise is one of those preconditioning stresses and exposure to heat is another.
Combining training with a hot environment could potentially be beneficial for performance, providing a protective thermotolerance effect against any subsequent heat stress during exercise. Share on XCombining training with a hot environment could potentially be beneficial for performance, providing a protective thermotolerance effect against any subsequent heat stress during exercise. This is because the combination of exercise and heat exposure can cause greater expression of HSP than either treatment alone. A recent study has approached this reflection from a new angle, suggesting that whole body heat stress after training additively improves endurance training-induced mitochondrial adaptations in skeletal muscle.3
In other words, post-exercise heat exposure increases physiological adaptations. Basking in a warm post-workout environment increases blood flow to the skeletal muscles, keeping them supplied with glucose, fatty acids, and oxygen while removing by-products of the metabolic processes.
When heat exposure becomes a routine, this hyperthermic conditioning reduces the use of muscle glycogen by a whopping 40% to 50%, possibly due to the increased blood flow to the muscles. One study has shown that a 30-minute sauna session twice a week for three weeks after training increases the time it takes for participants to run to exhaustion by 32%.4 This improvement in performance is accompanied by a 7.1% increase in plasma volume and a 3.5% increase in the number of red blood cells. More red blood cells equal increased oxygen supply. Heat acclimatization increases the number of red blood cells through erythropoietin (EPO) because the body tries to compensate for the corresponding increase in plasma volume.
Heat Exposure and Hypertrophy Gains
The benefits of heat exposure as a post-exercise recovery method don’t stop with endurance performance. Exercise can induce muscle growth. Heat induces muscle hypertrophy. Put in synergy, they induce hyper-hypertrophy. Heat acclimatization reduces the amount of protein breakdown and increases net protein synthesis and, as a result, muscle hypertrophy. Perhaps neither endurance nor hypertrophy is important to your sport? No problem. Heat therapy provides better post-workout recovery with three other notorious effects:
- Prevention of protein breakdown.
- Massive increase in growth hormone release.
- Improved insulin sensitivity.
Oxidative stress is a main cause of protein degradation. For this reason, any means that can prevent exercise-induced oxidative damage and repair damaged proteins, while maintaining exercise-induced protein synthesis, results in a marked increase in protein synthesis (anabolism). Intermittent heat exposure elicits a hormetic response (a protective response to stress) in which secreted HSPs work to prevent damages by directly removing free radicals and supporting cellular antioxidant capacity through their effects on glutathione maintenance. HSPs, moreover, repair misfolded and damaged proteins, thus ensuring the structure and function of muscle cells.
Hyperthermia and Growth Hormones Release
Hyperthermal conditioning increases anabolism and promotes recovery through massive induction of growth hormone. Many of the anabolic effects of growth hormone are primarily mediated by IGF-1, which is synthesized in response to growth hormone. There are two important mechanisms by which IGF-1 promotes skeletal muscle growth: It increases protein synthesis through activation of the mTOR pathway, and it decreases protein degradation via inhibition of the FOXO pathway. An increase in circulating IGF1 levels is associated with improved recovery after intense exercise, accelerated tissue regeneration, and increased performance in strength and power.
Exogenous administration of growth hormone and IGF1 is prohibited by WADA, and it is an offense to possess them. In the event of injuries or exacerbated fatigue, or even to speed up muscular adaptations to training, there’s no need to forge solid links with such and such cartel supplying prohibited products! Two 20-minute sauna sessions at 80 degrees Celsius separated by a 30-minute cooldown period results in growth hormone levels twice as high as the initial value.
Meanwhile, two 15-minute sauna sessions at 100 degrees Celsius interspersed with a 30-minute cooldown period increases growth hormone levels fivefold.
What is perhaps more surprising, however, is that repeated exposure to intermittent whole-body hyperthermia has an even more profound effect on stimulating growth hormone. One study shows that immediately after two one-hour sauna sessions a day at 80 degrees Celsius for seven days, starting on the third day, growth hormone levels were 16 times higher than pre-study levels.5 The effects of growth hormone usually persist for a few hours after the sauna.
It is also important to note that the combination of hyperthermia and exercise induces a synergistic effect on growth hormone. Inviting your athlete to relax in the sauna after a hypertrophy session can boost the muscle mass and strength gains even further. More results without the need for more repetitions means less fatigue and better performances in the long run.
Heat Exposure’s Effect on Insulin
Intermittent exposure to heat stress can also have an impact on the production and sensitivity of the insulin hormone. Insulin resistance is a common problem in athletic populations—especially in explosive sports—resulting in impaired glucose uptake and diminished performances. Resistant, diabetic mice were subjected to 30 minutes of hyperthermic treatment, three times per week for 12 weeks. Researchers reported a 31% decrease in insulin levels and a significant reduction in blood sugar, suggesting re-sensitization to insulin.6
Of course, your athletes are not exactly like obese, diabetic mice (at least, I hope not). However, the mechanism by which heat exposure affects insulin also applies to them. Hyperthermal therapy specifically targets skeletal muscle by increasing the expression of a type of transporter called GLUT 4, which is responsible for transporting glucose into skeletal muscle from the bloodstream. Decreased absorption of glucose by skeletal muscle is one of the mechanisms leading to insulin resistance. Heading straight to the post-workout sauna helps ensure optimal glucose transport to the muscle and decreases muscle breakdown—a winning combo that helps optimize recovery.
Heading straight to the post-workout sauna helps ensure optimal glucose transport to the muscle and decreases muscle breakdown—a winning combo that helps optimize recovery. Share on XImmediate, post-workout heat exposure strengthens the immune system, increases muscle adaptations, and improves aerobic performance. It guarantees a life-saving anabolism for muscle mass and the integrity of muscles, tendons, and ligaments, while optimizing insulin sensitivity, restoring muscle glycogen reserves, and stopping the degradation of cellular proteins. It’s difficult to name a recovery strategy that offers more benefits—and when we compare this list to the supposed effects of the cold, we understand that the sauna is often preferable to the ice bath.
What About Contrasts?
Cold has its advantages; hot has its own. Logically, there is a strong temptation to combine them to win on both counts. The “contrast” technique—changing from cold to hot and then from hot to cold over several cycles of varying lengths—is widely used as a post-workout recovery method in team sports.
Subjectively, this practice is the most enjoyable for the majority of athletes. On the other hand, physiologically, it is not that easy to kill two birds with one stone. Indeed, if prolonged exposure to cold and heat is able to change muscle temperature, this is not the case with contrast where only a fluctuation in body temperature has been reported. Studies on the potential benefits of contrast therapy on recovery post strenuous exercise are rather equivocal, with the main positive findings being a stronger muscle-swelling reduction when compared to passive recovery. However, studies looking at contrast versus cold water immersion therapy are rare, and all conducted so far show both types of immersion therapy induce superior recovery than just doing nothing, without one being much more potent than the other.
In a review of the different immersion therapies, Ian Wilcock, John Cronin, and Wayne Hing suggest that the majority of the benefits of such recovery strategy come from the hydrostatic pressure of the water, independent of the choice of temperature.7 If we stick to these conclusions, as long as your athletes casually wade for several minutes, going from hot bath to cold, the benefits will be the same regardless of the temperatures used. The physiological effects of contrast baths for the treatment of injuries have been well documented, but their physiological rationale for improving recovery is less clear.
Most of the experimental evidence suggests that immersion in hot and cold water helps reduce injuries in their acute stage, through vasodilation and vasoconstriction, thereby stimulating blood flow and reducing swelling. This blood-bypassing action may be one of the mechanisms for eliminating metabolites, repairing exerted muscle, and slowing metabolic processes.
While mild, benign, and probably quite positive, hot- and cold-water immersion is not a substitute for long-term exposure to cold or heat. Share on XTo date, very few studies have focused on the effectiveness of hot- and cold-water immersion for post-exercise treatment. While mild, benign, and probably quite positive, this recovery strategy is not a substitute for long-term exposure to cold or heat. The comfort of contrast baths makes them a consistent choice for following a session of low-to-moderate intensity and volume, or for fit players who don’t need a lot to get ready session after session.
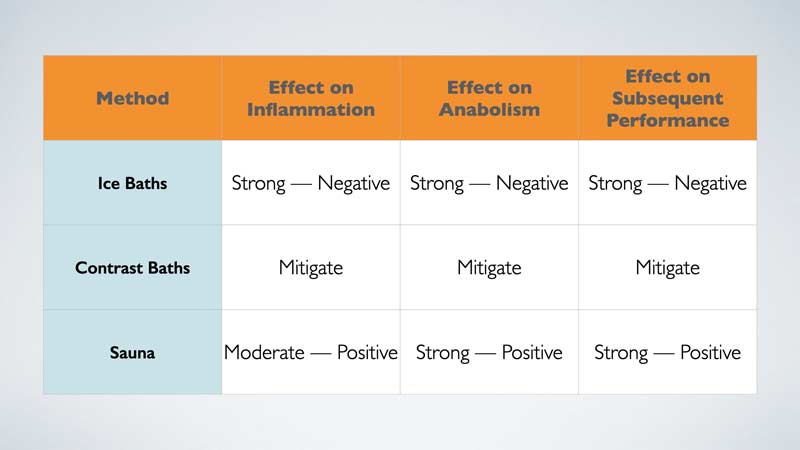
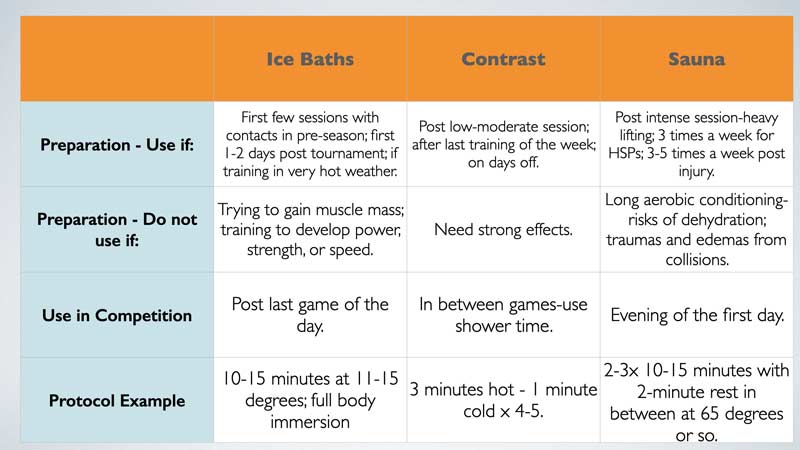
So, in the face of such a quantity of information, it may seem kind of difficult to make the right decision as to when to turn up the heat or immerse in the cold. Hopefully the charts below can offer an easy guideline when in doubt.
Since you’re here…
…we have a small favor to ask. More people are reading SimpliFaster than ever, and each week we bring you compelling content from coaches, sport scientists, and physiotherapists who are devoted to building better athletes. Please take a moment to share the articles on social media, engage the authors with questions and comments below, and link to articles when appropriate if you have a blog or participate on forums of related topics. — SF
References
1. Roberts LA, Raastad T, Markworth JF, et al. “Post-exercise cold water immersion attenuates acute anabolic signalling and long-term adaptations in muscle to strength training.” The Journal of Physiology. 2015;593(18):4285-4301.
2. Higgins T, Greene D, and Baker M. “Effects of Cold Water Immersion and Contrast Water Therapy for Recovery from Team Sport: A Systematic Review and Meta-analysis.” The Journal of Strength and Conditioning Research. 2017;31(5):1443-1460.
3. Gryka D, Pilch W, Szarek M, Szygula Z, Tota Ł. “The effect of sauna bathing on lipid profile in young, physically active, male subjects.” International Journal of Occupational Medicine and Environmental Health. 2014;27(4):608-618.
4. Mero A, Tornberg J, Mäntykoski M, and Puurtinen R. “Effects of far-infrared sauna bathing on recovery from strength and endurance training sessions in men.” SpringerPlus. 2015;4:321.
5. Kukkonen-Harjula K and Kauppinen K. “Health effects and risks of sauna bathing.” International Journal of Circumpolar Health. 2006;65(3):195-205.
6. Scoon GS, Hopkins WG, Mayhew S, and Cotter JD. “Effect of post-exercise sauna bathing on the endurance performance of competitive male runners.” Journal of Science and Medicine in Sport. 2007;10(4):259-262.
7. Wilcock IM, Cronin JB, and Hing WA. “Physiological response to water immersion: A method for sport recovery.” Sports Medicine. 2006;36(9):747-765.


Does heat provoke vagus nerve stimulation as well as cold? I find cold (or contrast heat-cold) better than just heat for the subjective feeling of calm/relief from vagus stimulation
After sauna after hypertrophy training I take a cold (not ice) bath to cool back down to a normal body temperature. Is this bad for gains?