Breath mechanics are at the literal core of the human body. Most obviously, they have a direct effect on the air coming in and going out of the body, but much more is going on. So much so that perturbed breath mechanics create a ripple effect that holistically and simultaneously impacts neurological, motor, and psychoemotional systems.
If coaches and athletes better understand how far-reaching the positive and negative effects can be, I’m sure that far more attention would be paid to teaching good breathing habits and alleviating poor ones. Even slight changes in breathing can yield significant long-term results—reaching far beyond the obvious and with a relatively low cost in time and effort.
If coaches and athletes better understand how far-reaching the positive and negative effects can be, far more attention would be paid to teaching good breathing habits and alleviating poor ones. Share on XConversely, compensatory and dysfunctional breathing mechanics in athletes have multiple adverse downstream effects on performance. Training for and competing in sports is stressful on the human body, and combining the repetitive and lopsided demands of all sports will create compensation. These effects are subtle and can be difficult to prioritize in the scheme of problems coaches face. Left unchecked, however, breathing compensations can aggregate like interest on an unpaid debt.
The goal for us as we study this subject here is to develop a basic understanding of the holistic nature of breath pattern dysfunction in athletes, some of the limitations it causes, how it presents itself on the field of play or in training, and what we can do about it within our scope of practice.
Athletic Breathing Dysfunction Overview
Let’s make sure we are crystal clear about what dysfunctional breathing is. It is “Inappropriate breathing which is persistent enough to cause symptoms, with no apparent organic cause” (Cliftonsmith & Rowley, 2011). This means that the athlete does not have an underlying disease state of which poor breathing may be an expression: for example, a metabolic disorder like diabetes that may cause a higher offload of energetic waste. Since many of these disorders are non-factors for athletic populations, most breathing issues can be attributed, at least in part, to poor mechanics.
As a point of conscience, though—if you have an athlete who consistently can’t breathe, send them to medical care!
The symptoms of poor breathing can be hard to spot because they can be situational and sporadic. However, breathing dysfunction can surface as shortness of breath during activity (duh), frequent yawing/sighing, chest and upper back pain, air hunger (“can’t catch my breath”), unusual fatigue, and anxiety/panic attack (this one is especially important in modern youth athletics).
The symptoms of poor breathing can be hard to spot because they can be situational and sporadic. But the energetic costs for poor breathing can aggregate. Share on XAdditionally, negatively altered breathing mechanics can result in altered motor patterns downstream that disrupt postural orientation as well as extremity coordination. Long-term hyperinflation patterns can result in poor length-tension relationships in trunk muscles and put undue stress on postural muscles in the low back especially. Poor breathing also does the obvious: you bring in less oxygen/per unit breath (aka vital capacity). In other words, you’re shallow, Hal. Last but not least, aerobic efficiency can become enfeebled over time, and energetic costs for poor breathing can aggregate.
The nature of the human body is so completely interwoven and interrelated that it can be difficult to say with absolute precision that “X issue” equals “Y problem.” However, identifying areas of emphasis can help coaches better understand the components of complex systems in a way that allows for better problem-solving and application of interventions.
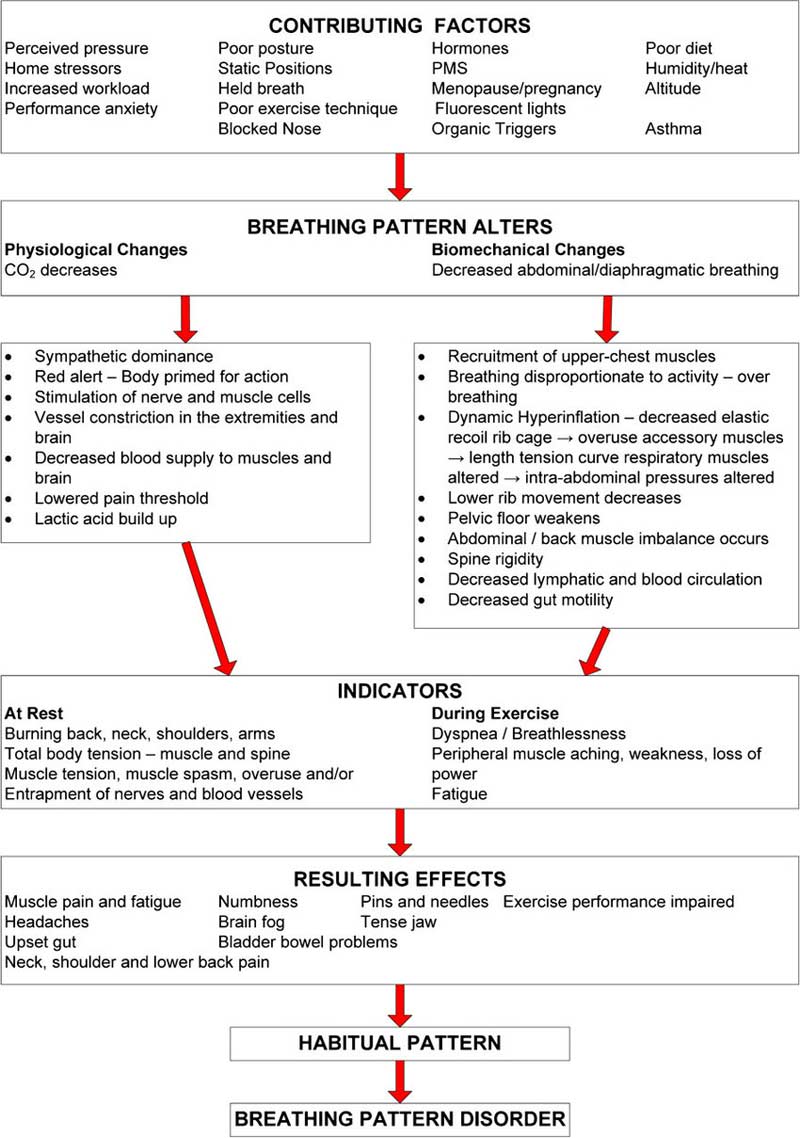
Because ventilation is a foundational component of human anatomy and physiology, many things can cause and contribute to disordered breathing (and vice versa). More than just poor mechanics contribute to breathing disorders—everything from pain, autonomic arousal, and sinus dysfunction to pregnancy and diet can contribute to the etiology of breathing issues. Regardless of origin, the continuum of effects of altered breathing is varying degrees of physiological, psychoemotional, and biomechanical outcomes.
The best way to begin attacking these issues is by first identifying the ideal and moving toward that ideal with progressive skill. Don’t get too lost in the corrective weeds and steal all the fun from the sports physios out there.
Keep It Super Simple
All roads lead to Rome. Regardless of where an athlete’s breathing problems come from—or the direction they’re going—there has to be a mechanical change to elicit a positive response. This means that there’s a change in movement skill at the most fundamental level, and that’s where coaches live.
If you’re a coach, rather than focusing on the minutiae of correctives, use simple mechanical tools that athletes can learn and repeat accurately. Share on XThere is a vast literature on the many positive effects of “diaphragmatic breathing” as well as “chest breathing” and the negative ones. If you’re a coach, rather than focusing on the minutiae of correctives, use simple mechanical tools that athletes can learn and repeat accurately. As my friend Mickey Schuch says: “Is it robust? Is it reliable? Is it repeatable?”
A Word on Cueing
When I hear things like “use your diaphragm,” my neck hair stands on end a little. No coach worth their salt would ask you to run faster by “using your rectus femoris.” Instead, we provide cueing that gives a point of focus and movement instructions (constraints) that allow the athlete to envision the end result and then start iterating. It’s the same with breath mechanics.
Have an accurate and reliable ideal that you will use as a measuring stick. Most generalist coaches have neither the time nor the inclination to become breathing experts. However, a basic understanding is a must because of the breadth and depth of both the harm and the benefit from breathing.
A basic understanding of breath mechanics is a must because of the breadth and depth of both the harm and the benefit from breathing. Share on XIn that vein, let’s touch a little bit on identifying and cueing ideal mechanics—for the sake of brevity, we’ll cut right to the chase. (If you are looking for a more detailed reference on breath mechanics, check out this article.)
Three steps to keep it super simple:
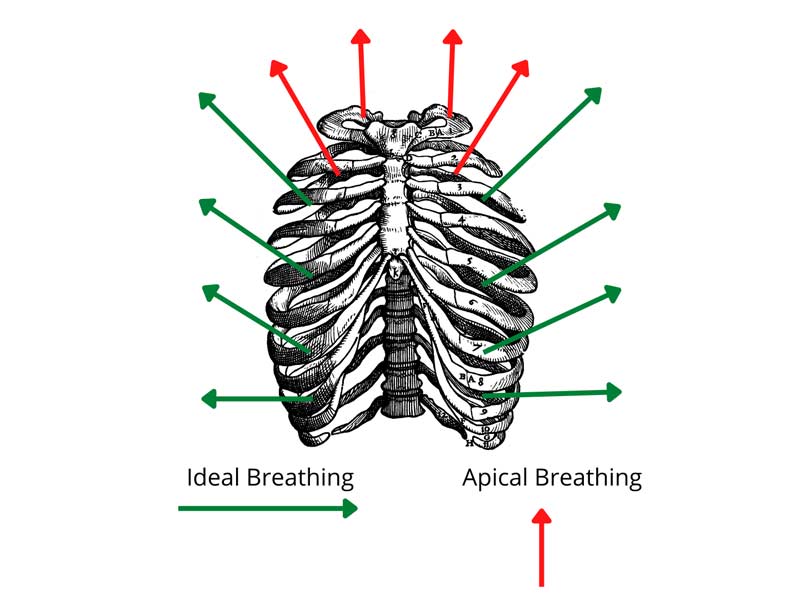
- Cue the ribs. Learn to move ribs, not bellies. Athletes brace their trunk position to deal with higher forces on their structure, so moving the belly is not a viable option under many circumstances, especially competitive ones.
- Fill the bucket. Ribs should move in waves from bottom to top as well as up to the sides just like filling a bucket with water.
- Control the flow. Imagine sipping air slowly through a straw (but with your nose). If you try to suck everything in at once, the straw will collapse. Keep the flow smooth and deliberate.
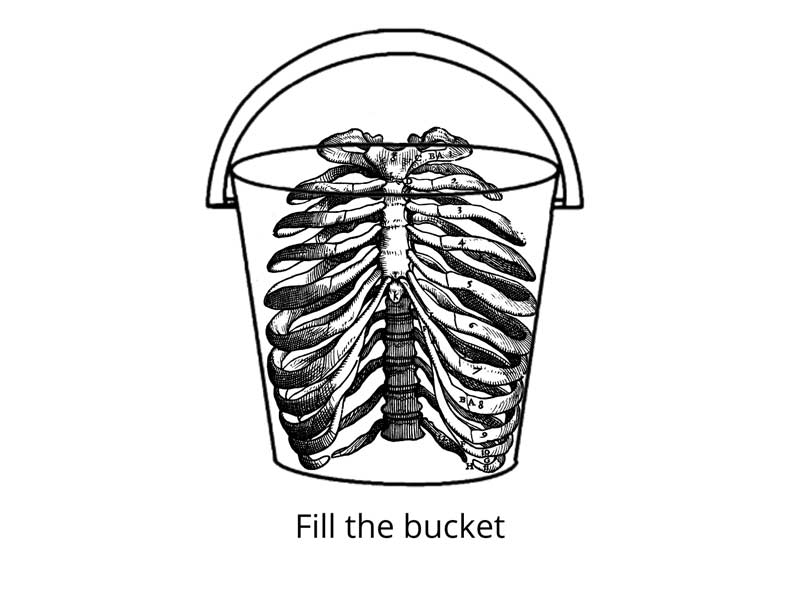
These three principles will help orient athletes toward breathing that primarily uses the diaphragm and intercostals while using accessory breathing muscles as, well, accessories. When you see breathing like this, the ribcage moves smoothly and evenly all the way around the torso. As we’ll discuss in more detail, the demands of athletics have some compensatory and dysfunctional patterns that can be easily redirected with simple, well-applied tools.
Video 1: Learn how to cue ideal mechanics before introducing any potential corrections.
As a final reminder: it’s easy to get stuck in the correctives without practicing the movement well and often. Use the ideal mechanics as a benchmark before and after any intervention, so you know if you’ve made a change.
Regardless of origin, you can alter breathing habits toward the positive with mechanical interventions that don’t require specialized expertise. The easy way to stratify these is through lower-body- and upper-body-focused interventions.
Lower Body Interventions
It might seem like the lower body has less implication for breathing mechanics and that improving them may not have much effect on issues in this area. Not at all. Well-implemented breathing strategies can dramatically and positively affect outcomes for lumbopelvic dysfunction. It may be truly impossible to separate the mechanical from the holistic outcomes of improved diaphragm engagement, but let’s start there.
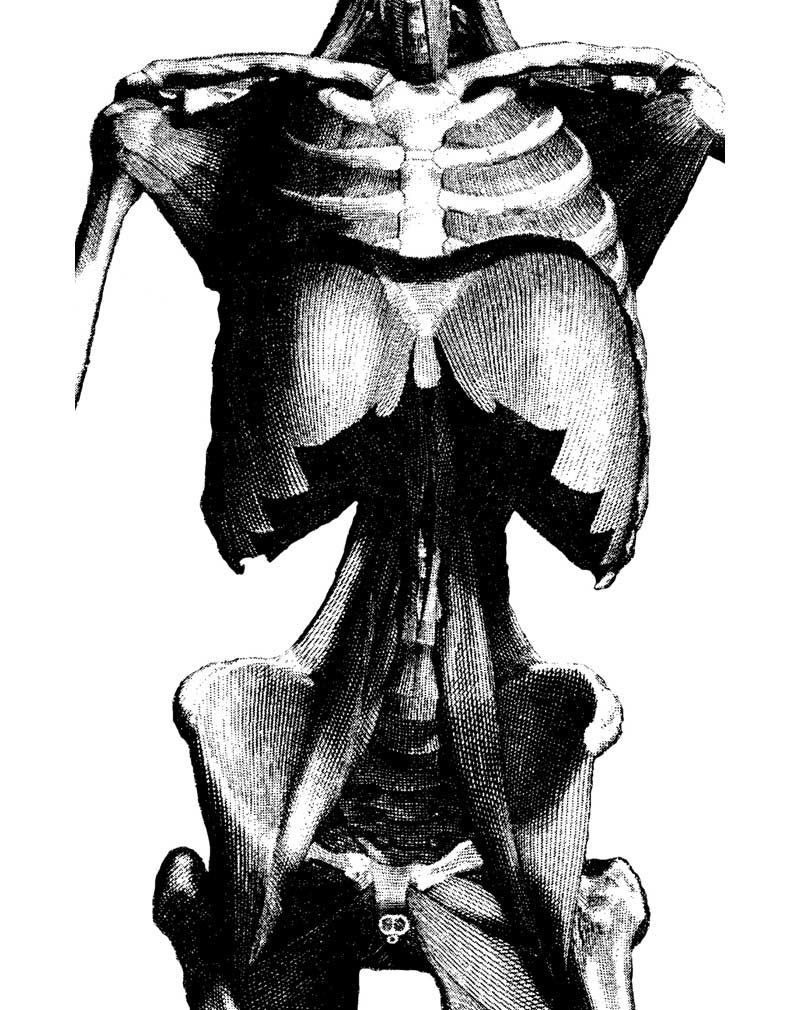
Athletes who, through genetic anthropometry or movement history, develop local extension moments in the lumbosacral area often have increased tone in deep hip flexors that can put undue stress on the system and limit diaphragm excursion. Contrary to popular belief, athletes with a proclivity for spinal extension will not snap in half at the first sign of trouble. So, it’s important we alter our thinking from one of correction to one of integration. Is the system working together optimally? Is one spot stealing efficiency from another?
Contrary to popular belief, athletes with a proclivity for spinal extension will not snap in half at the first sign of trouble. It’s important we alter our thinking from correction to integration. Share on XThe psoas and the diaphragm share some important anatomy with serious implications for not only better breathing but also spine and hip function. The bottom of the diaphragm, called the crura, comes down like snake fangs between T10 and T12 and crisscrosses with the upper and medial portions of the iliopsoas, continuing upward toward the spinal origin of the diaphragm. Of course, also woven in are the usual suspects: QLs, transverse abdominis, latissimus dorsi, and the other members of the paraspinal gang. Most importantly, all that tissue interlocks with the thoracolumbar junction and acts like a Chinese finger trap to mechanically reinforce that area of the body.
The first lower body intervention we’re focused on here is a kind of pelvic “tempering” (a term coined by the legendary Donnie Thompson). Here we use direct pressure into the iliopsoas with hip and leg extension to deal with tissue stiffness. Due to the anatomical relationship with the breathing mechanism described above, maintaining smooth, controlled breathing is an absolute must to maximize this technique. If it feels like it’s too much, back off or stop.
Video 2. Iliopsoas Tempering.
The second lower body intervention is the classic deadbug, but with some applied nuance. Here we emphasize lumbopelvic positioning with breathing added in. This “core” exercise can be valuable if done with attention and intention instead of the lackadaisical approach of an actual dead bug that is all too common in even the fanciest training halls. Pressurize the trunk using the cueing from above and then move the hip into relative extension without creating local movement at the spine. This technique reveals some nuanced connections in the kinetic chain while at the same time creating a therapeutic input.
Video 3. Deadbug
These exercises can be used separately or in a superset fashion. I’ve had the most success with the latter application. The first technique creates some options for movement, and the second dials in the software. Going back and forth with low but focused repetitions gives the athlete a feel for the breathing’s new range and application without getting overwhelmed.
Application
Alternate
- 1:00–2:00 body tempering/side (with 3–5 reps leg extension).
- 6–10 deadbugs: Slow and controlled! Set posture, nasal inhale (fill the bucket), extend leg, return leg, nasal exhale.
Key Points:
- These exercises are subtle, not passive. Keep your and your athlete’s attention locked on the details.
- Do not approximate an arbitrary range of motion. Focus on the constraints given in the video to maximize the outcomes.
- Make the breath the center of the focus for the exercises and everything else secondary.
The lower body techniques described here are not intended as a panacea by any means, but they can move the needle on essential pieces of the breathing puzzle. I’ve found these exercises incredibly beneficial for not only helping athletes reset faulty breathing mechanics but also helping to create a more integrated relationship between the tissues around the trunk and the ability to manage pressure. This enhances overall stability and can diminish negative feedback from pain-sensitive tissues and increase mechanical breathing efficiency.
Bonus Technique: Super Lunge
You want to be super, don’t you? Good. Pay attention to the details of this exercise, and you will be.
Video 4. Super lunge: The basic lower body interventions use breath and movement together to progressively improve the coordination of the trunk to deal with force inputs more efficiently.
Upper Body Interventions
Athletes, in particular, often suffer from “hyperinflation” issues stemming from apical breathing. Apical breathing is when the mechanical load for ventilation is adversely distributed to the accessory muscles of the chest and shoulders. This cycle often results in poor and partial exhalation preventing the full contractile cycle of the diaphragm. Over time, this, combined with other mechanical inputs, can create aggregate compensations and potentially true dysfunction. These can limit performance through their contributions to mechanical issues in the upper body but also by restricting optimal energetic efficiency that is managed by breathing.
Most of the time, when we think of neck and shoulder problems, in particular, improving breath mechanics does not come to mind as a solution. However, simple interventions that improve breath mechanics have both holistic and direct mechanical benefits, specifically for issues in the neck and shoulder. Holistically, removing roadblocks to breathing efficiency takes the edge off the nervous system, yielding a net benefit to any movement strategy that may be used body-wide.
Simple interventions that improve breath mechanics have both holistic and direct mechanical benefits, specifically for issues in the neck and shoulder. Share on XAdditionally, many accessory breathing muscles have crossover functions in the upper body, the most obvious being the scalene, sternocleidomastoid (SCM), and pec major and minor. These muscle groups implicated in neck and shoulder dysfunction frequently have a breathing pattern disorder as an associated causal factor. Conversely, neck and shoulder dysfunction affects downstream breathing pattern issues.
Our first upper body intervention is to help bring awareness to and encourage the full range of motion in the ribcage. This includes the global sense of thoracic extension and rotation but also the more granular relationships of the ribs to each other. Larger tools like rollers tend to encourage global extension. To get more precise, a smaller fulcrum is necessary. For this, you can use a cheaper and more ubiquitous tool like a lacrosse or tennis ball or get something specifically designed for refined t-spine access.
Video 5. T-spine opener.
Key Points:
- Be purposeful. Don’t just slide all over the place like you’re getting moved down an assembly line.
- Use breath first. A full inhale will create pressure and traction in the area first.
- Pops don’t mean it’s working. Your indicator shouldn’t be that your spine sounds like a crackling campfire. Sometimes it does; sometimes it doesn’t. Can you breathe/move better?
The second upper body intervention is the neck peel. This is simply using a tool to create drag over the SCM and other regional tissues to relieve tension associated with apical breathing and neck/shoulder dysfunction. This technique is all about using the ball to wind up superficial fascia. This can be done almost anywhere, whether seated or standing, and in my experience, it gives tremendous relief from a variety of issues.
Video 6. Neck Peel.
Key Points:
- Go slow. Three seconds to move an inch is a good rule of thumb.
- Create drag. Grab and slide the tissues; don’t push into the neck.
- Explore and move. Start with the traditional origin and insertion, but remember that the systems are interconnected. Go where things are sticky.
Some final words on applying these tools. Repetition over intensity: your athlete should be able to control their breathing the entire time. Order matters: do the steps given in the video in order—every time. The given order emphasizes tissues in very specific ways, so don’t just wing it.
Performance Anxiety
While performance anxiety doesn’t have as obvious of a mechanical cause as some of the issues we’ve already discussed, understanding the part that breath plays is essential for helping athletes on your roster who may suffer from this issue. Furthermore, it gives coaches and athletes access to a solution that is:
- Free of stigma.
- Accessible anytime and anywhere, whether in the field of play or not.
- Within a coach’s wheelhouse.
Performance anxiety has multifactorial origins, and breathing dysfunction—while not the sole cause—usually plays some part in the propagation of performance-related anxiety. That said, there are definitely signatures patterns of shallow, inhale-focused breathing that cause dysregulation in carbon dioxide levels. Over-arousal of the autonomic nervous system expresses itself as anxiety on the psychoemotional level but as breathing dysfunction on the physiological level. This increased arousal response acutely upregulates the urge to breathe. Those suffering from performance anxiety are often referred to as “stuck on the inhale.” This means that they’re breathing in the upper part of the ribcage with the muscles of the neck and shoulders.
Breathing dysfunction usually has some part in performance anxiety. Making breathing the focal point turns what can be a hard-to-grasp problem of the mind into a physical skill the athlete can learn. Share on XSelf-perpetuation of these habits through behavioral-psychological-physiological loops can be interrupted by pulling on the lever of breathing. Making breathing the focal point turns what can be a hard-to-grasp problem of the mind into a physical skill the athlete can learn. This is really empowering because athletes know how to learn physical skills!
Video 7. Breathing intervention for performance anxiety.
When performance anxiety hits the breathing, symptoms tend to come as short repetitive urges to inhale. Trying to “take a deep breath” at that point can actually worsen the feeling of panic. Instead, “catch the exhale” by pushing air out with short, controlled bursts and then slowing things down progressively.
Think of it the situation as two spinning gears. One gear is the athlete’s anxious state: it’s spinning at 1,000 RPMs. The other gear is breathing. If you bring that gear in at 100 RPMs, they’re too far apart, and they’ll just grind each other up. Catching the exhale is like bringing the catch gear in at 950 and then slowing the whole thing down together. Pump the brakes—don’t smash them.
One more thing: Stop. Just stop. Unless your athlete has something life-changing on the line in this game or practice, have them discontinue play and regain their composure. The headlines are chock full of athletes who have pushed through mental health issues at a serious personal cost. No need to add to that pile.
Additionally, this generally moves away from thinking of athletes as commoditized sports robots and acknowledges that there’s a human being in front of you. This approach will undoubtedly build trust between you and your team on a deeper and more meaningful level.
Not the One but the Many
When it comes to an issue that has the potential to reduce function and efficiency system-wide, it behooves coaches to take notice and minimally learn the basics. Breathing pattern dysfunction is broad-reaching and nefarious. There is rarely a moment of catastrophic collapse. In most cases, they slink in slowly, under the radar. A little too much mouth breathing here, a little back or neck pain there, a bit more use of the inhaler, mix in some pre-game anxiety, and you have a nice little cocktail of issues that can put serious limits on athlete health and performance over the long haul.
It’s not one big swing of the axe. It’s death by a thousand cuts.
Since you’re here…
…we have a small favor to ask. More people are reading SimpliFaster than ever, and each week we bring you compelling content from coaches, sport scientists, and physiotherapists who are devoted to building better athletes. Please take a moment to share the articles on social media, engage the authors with questions and comments below, and link to articles when appropriate if you have a blog or participate on forums of related topics. — SF
Resources
Bahr R, Andersen SO, Løken S, Fossan B, Hansen T, and Holme I. “Low back pain among endurance athletes with and without specific back loading—a cross-sectional survey of cross-country skiers, rowers, orienteerers, and nonathletic control.” Spine. 2004;29(4):449–454.
Bradley H and Esformes J. “Breathing pattern disorders and functional movement.” International Journal of Sports Physical Therapy. 2014;9(1):28–39.
Cliftonsmith T and Rowley J. “Breathing Pattern Disorders and Physiotherapy: Inspiration for Our Profession.” Physical Therapy Reviews. 2011;16(1). doi:10.1179/1743288X10Y.0000000025
Hodges PW, Eriksson AEM, Shirley D, and Gandevia SC. “Intra-abdominal pressure increases stiffness of the lumbar spine.” Journal of Biomechanics. 2005;38(9):1873–1880.




