“Water makes you weak…”
Many of us who work in the sports industry and are of a certain age have a real-life horror story about hydration reminiscent of that scene with Coach Boone (masterfully portrayed by Denzel Washington in Remember the Titans). Thankfully, attitudes and guidelines about hydration, performance, and recovery have changed markedly over the past 40 years. Hydration breaks aren’t just modern staples of practice, they are now being included as part of game day operations for major sporting competitions at many levels of sport.
All of this is for good reason, as governing bodies of sport across the globe understand the importance and health and safety aspects of hydration. As a result, athletic trainers, sport nutritionists, and other allied health and performance staff members have taken an interest in encouraging better hydration behaviors among athletes. There are times of the year when suboptimal hydration can not only impact performance but also put lives at risk.
Having worked in professional and collegiate athletics myself—and knowing staff members in multiple leagues and levels across sports—I can attest firsthand to the level of investment that organizations make to help support athlete hydration. Annual bottled-water budgets alone can soar above $20,000 for a team of about 30 athletes—a separate cost from any other sports drink or hydration-related supplement. A team located in a region where tap water is of poor quality can expect to invest heavily in bottled water, on top of “hydration stations” and fountains around facilities. I spoke with a head athletic trainer from the NFL this past year who submitted a yearly budget with over $120,000 for hydration and hydration-related supplements for his roster.
Annual bottled-water budgets alone can soar above $20,000 for a team of about 30 athletes—a separate cost from any other sports drink or hydration-related supplement, says @MdHCSCS. Share on XProfessional teams aren’t the only ones investing in hydration at staggering rates. As of 2019, top collegiate athletic departments were spending nearly $60,000 each year on the equivalent of 21,000 gallons of sports drinks to help hydrate their athletes. In fact, the investment in hydration is only a portion of a larger budget aimed at fueling athletes for performance and recovery. Universities devote millions of dollars each year to fuel athletes, and much of this is made possible by an NCAA rule change in 2014 that allowed schools to support the nutritional needs of many more athletes within their department.
Hydration-related products are only part of the puzzle, as equipment and sports technologies also take up a sizeable portion of athletic training and performance department budgets. Despite budget cutbacks, recent surveys among collegiate and professional athletic trainers and performance staff show 44% of teams surveyed spend a minimum of $50,000 per season on sports technology monitoring aspects of health and performance. In addition to professional settings, these big budgets are nothing new at universities here in the United States, particularly in their football programs.
Despite big investments in the fueling aspect and the known impact on performance and health and safety, hydration monitoring budgets and methods in particular have largely lagged behind.
Hydration for Health and Safety
The hefty budgets devoted to hydration are justified, as fluid intake plays a big role in maintaining the health, safety, and performance of athletes. Ask any athletic trainer who has worked during the summer how often they push athletes to hydrate, and you will likely get a smile and an eye roll. Their efforts are for good reason, as NATA position statements have raised awareness around the fact that more than half of high school, collegiate, and professional athletes begin an activity while dehydrated. This is concerning from a safety standpoint, as dehydration—combined with physical exertion during activities in warm weather—reduces the ability to regulate core body temperature and subsequently greatly increases the risk of heat-related illnesses. Tragically, heat illness is one of the leading causes of death among high school athletes and has contributed to more than 30 deaths of collegiate football players since 2000.
While the magnitude of the importance of adequate hydration for athletes seems to center around focusing efforts during warm weather spells, the impact of hydration plays an important role for all athletes year-round. Dehydration has a significant impact on the body and subsequent performance output.1–4 While muscle cramps and sluggishness in the later stages of practices and competition were once thought of as prime examples of decreases in performance, more recent research reviews have widened our understanding of the issue.
Hydration and Performing Sports Skills
Barnes & Baker (2021) completed a comprehensive research review of literature focusing on the impact dehydration has on cognition, sport-specific skills, and physical performance. Twenty-two of 34 studies reported dehydration as having a negative impact on cognition, skills, and physical performance in sports such as basketball, soccer, American football, and others.
The negative impacts of dehydration were pronounced when body mass deficit exceeded 2%, especially when combined with stress from heat. Of all the elements examined, 71% of the studies focusing on cognition reported decrements in cognitive performance due to dehydration. An additional 67% of the studies included in this review found dehydration to have a negative impact on sport-specific skills.
Nuccio et al., (2017) completed a similar comprehensive review of literature focusing on the impact of dehydration on cognitive, technical, and physical performance in sports. This review further focused on the cumulative impact of dehydration on cognition, technical skills, and physical performance as well as the effect on team sport performance. Results were mixed from sport to sport, given differences in rehydration opportunities unique to passages of play across sports; however, similar findings were reported regarding negative effects of dehydration on cognition, technical sports skills, and physical performance.
The findings described above are not groundbreaking developments, but given the frequency stated earlier about how many high school, collegiate, and professional athletes train or compete on a daily basis while dehydrated, are we missing an opportunity to better prepare athletes for their sport? There are countless discussions, many in the form of the outstanding blogs posts and roundtables on SimpliFaster, that help elucidate paths forward in training and programming. As a field, we make consistent efforts to maximize the physical performance of each athlete through those training programs, yet we are now presented with the reality that athletes are unknowingly preventing themselves from reaping the full benefits of that work. How can we make the most of our work to support athletes?
Monitoring Hydration: Methodology
Monitoring hydration status can be a simple endeavor to help mitigate decrements in performance due to dehydration. While some clinical settings have identified plasma osmolality as a gold standard for assessing hydration, these and some other methods aren’t practical for all, given budget or staffing constraints.7
Monitoring hydration status can be a simple endeavor to help mitigate decrements in performance due to dehydration, says @MdHCSCS. Share on XIn applied settings, there are several commonly used approaches used to monitor hydration, and efforts should be taken to move beyond overly subjective methods that can lead athletes astray. Regardless of the approach, the underlying focus should center on actually helping athletes take action to stay on top of their hydration.
Weigh-Ins for Fluid Loss
Pre- and post-activity weigh-ins are a good indicator of fluid loss and can be implemented throughout most of the week. It is common for teams to tie this process into other activities surrounding body weight maintenance or as part of a baseline assessment during force plate testing. Issues around standardization are a key consideration here, and as someone who has personally performed well over 34,000 weigh-ins in a chaotic locker room environment (amateur numbers by the standards of seasoned athletic trainers and nutritionists/dietitians), I can attest firsthand that repeatability standards can suffer greatly regardless of which staff is present.
It’s important to remember that weigh-ins only tell part of the story around hydration status, as sweat rates causing fluid loss can be highly individual, and the day-to-day trends can vary depending on the fed-status of the athlete. Given issues around reproducibility, as well as recent high profile issues around misapplication of this data, it is wise to exercise prudence in how these are implemented in order to optimize their impact.
Bio-Impedance for Body Composition and Hydration
Those who already possess the technology can intertwine weigh-ins with body composition measurements on top of a relative hydration status. There are noted limitations with bio-impedance when it comes to assessing hydration status,5,6and given the aforementioned issues around misusing and abusing body composition data, any regular usage of this technology for the secondary purposes of hydration status may not be warranted. Additionally, this method can require staffing devoted to the process and a hefty investment in the technology itself.
Saliva Testing and Thirst
Saliva testing is seen as a minimally invasive hydration assessment and is typically a good proxy to thirst levels. This is particularly true during exercise and in high temperatures; however, there are noted individual variances observed in testing.8 From a practical standpoint, stopping athletes during training or immediately after a session will require dedicated staff support and athlete adherence, as well as the handling of bodily fluids. Even prior to the COVID-19 pandemic, most practitioners would admit to being less than enthusiastic about sample collection.
There are also noted issues with standardization in field testing, as athletes submitting samples at differing intervals between fluid intakes can skew results in some cases. Thirst itself is typically considered a strong subjective indicator, but it is also regarded as a sign that the athlete is already suffering from dehydration.
Sweat Rate Assessments: Patches and More
Assessing an athlete’s sweat rate and content can be done in the field using several techniques that include absorbent patches, apparel, towels, and other laboratory-grade tools. A portion of the sweat rate approach also relies on weigh-ins to factor in fluid loss, while the aforementioned tools used in the field are aimed at better understanding the electrolyte content of sweat. Sweat rate is highly individual, but it reflects what happens during any given activity and should be used in conjunction with objective measures of pre-activity hydration status.
Sweat rate is highly individual but reflects what happens during any given activity and should be used in conjunction with objective measures of pre-activity hydration status, says @MdHCSCS. Share on XBecause of high variability in sweat rate and electrolyte content, an individualized approach would be necessary as opposed to relying on generalizability from any one measurement to a larger group. Many methods typically require dedicated staff time to collect and analyze samples of bodily fluids, and immediate results may not be practical in field settings. However, the information from these assessments can be a critical part of better understanding individual trends in sweating and identifying the necessary and appropriate strategies for acute rehydration efforts.
Urine Color
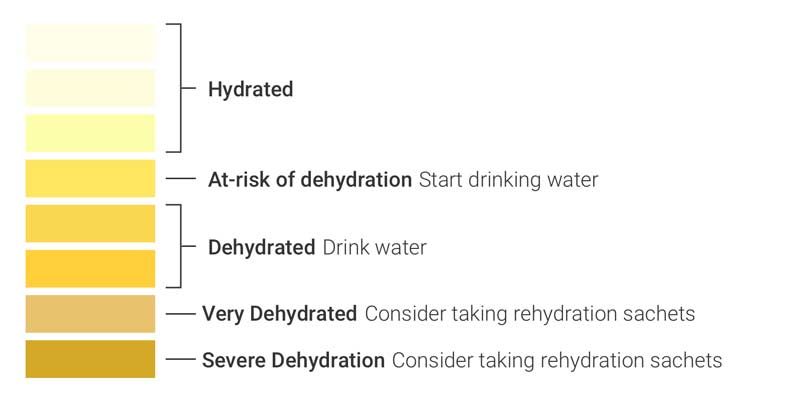
Perhaps one of the most widely adopted methods for assessing hydration status is the use of a urine color chart. Urine charts have been deployed at every level of sport, and they are intended to act as an easy-to-follow method for athletes to understand their hydration status. Interestingly, the validity of urine color charts has not been systemically evaluated in clinical settings, despite widespread adoption in athletics. While in theory urine color represents a proxy to hydration status, some studies that have used urine color in efforts to validate this proxy saw trained clinicians perform the assessment—not athletes.9
Urine sample charts, measured in arbitrary units (AU) 0-8 (10), are subjective in nature due to their dependence on athlete interpretation against a posted color chart. These charts can provide some assistance as a very low-cost alternative, as their intended use is for implementation where close estimates are acceptable. Urine color charts are not meant as a substitute for more accurate and reliable measurements.
Urinalysis (USG) Technologies
Urine Specific Gravity (USG) examines the density of urine against the density of water and is considered a good proxy to urine osmolality and overall hydration status in most cases.11 This approach is also considered the closest to a “gold standard” for non-clinical, field-based hydration status monitoring. Common instruments used by athletic trainers and sports nutritionists or dietitians are refractometers and dipsticks, with refractometers considered more reliable at assessing USG. USG is measured along a spectrum of 1.000 to 1.030+, where a widely accepted cut-off for dehydration is > 1.020.
The main issue with widely implementing this approach is the requirement of collecting and analyzing urine samples, which requires dedicated staffing time and effort, as well as relying on athlete compliance. While USG levels account for hydration status better than many field-based approaches, there are many user workflows in team settings where the athletes themselves aren’t made aware of their status prior to engaging in their athletic activities.
Intake Health has produced a first of its kind solution to help supplement these efforts, building field-leading, objective hydration monitoring into an athlete’s daily routine. This is paired with staff-customized infographics to help drive hydration behaviors to positively impact hydration status before activity. The InFlow hydration monitoring solution is a positive development, helping solve a critical problem for health and performance staff needing daily pre-activity hydration monitoring as part of their athlete fueling strategy.

Monitoring Hydration: Best Practice
There are several key takeaways to consider as staff forms their best practice approach to monitoring athlete hydration:
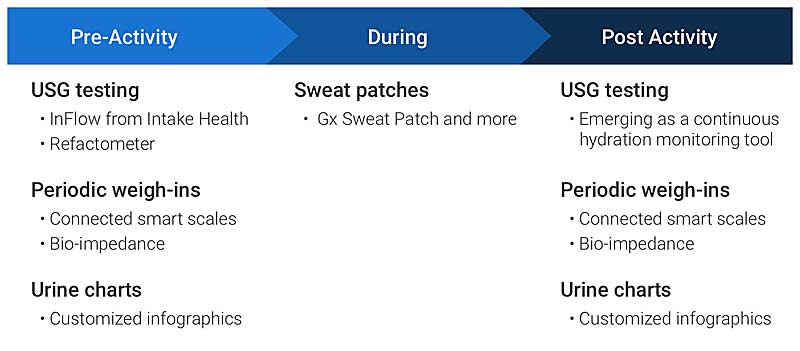
- There are no silver bullets in hydration monitoring, and good, reliable information is needed before, during, and after sports activities. Any one method used in isolation can inaccurately represent an athlete’s overall hydration status7—context is needed to help inform action.
- Hydration is important year-round and is an all-day event. Extra attention should be given during high temperatures and periods of heavy training (pre-season camps, excessive competition fixtures, etc.) as well as before, during, and after practice.
- Hydration monitoring procedures and refueling strategies must be impactful, related to each other, reproducible, minimally invasive to athletes, not require excessive staff time, and actually support a change in hydration behaviors. Advancements in technology are enabling procedures to achieve all of the above.
Consider the template below as a reference when designing or refining your team’s hydration monitoring strategies, with emphasis given to minimally invasive, accurate, repeatable processes.
Since you’re here…
…we have a small favor to ask. More people are reading SimpliFaster than ever, and each week we bring you compelling content from coaches, sport scientists, and physiotherapists who are devoted to building better athletes. Please take a moment to share the articles on social media, engage the authors with questions and comments below, and link to articles when appropriate if you have a blog or participate on forums of related topics. — SF
References
1. Sawka MN, Burke LM, Eichner ER, Maughan RJ, Montain SJ, and Stachenfeld NS. “American College of Sports Medicine position stand. Exercise and fluid replacement.” Medicine & Science in Sports & Exercise. 2007;39:377–390.
2. Armstrong LE, Casa DJ, Millard-Stafford M, Moran DS, Pyne SW, and Roberts WO. “American College of Sports Medicine position stand. Exertional Heat Illness during Training and Competition.” Medicine & Science in Sports & Exercise. 2007;39:556–572.
3. Kavouras SA. “Assessing hydration status.” Current Opinion in Clinical Nutrition & Metabolic Care. 2002;5:519–524.
4. Bernardot D. Advanced Sports Nutrition. Canada: Human Kinetics; 2006. p. 75–101.
5. Ugras S. “Evaluating of altered hydration status on effectiveness of body composition analysis using bioelectric impedance analysis.” Libyan Journal of Medicine. 2020;15(1):1741904. doi:10.1080/19932820.2020.1741904
6. O’Brien C, Young AJ, and Sawka MN. “Bioelectrical impedance to estimate changes in hydration status.” International Journal of Sports Medicine. 2002 Jul;23(5):361–366. doi: 10.1055/s-2002-33145. PMID: 12165888.
7. Barley OR, Chapman DW, and Abbiss CR. “Reviewing the current methods of assessing hydration in athletes.” Journal of the International Society of Sports Nutrition. 202;17,52.
8. Villiger M, Stoop R, Vetsch T, et al. “Evaluation and review of body fluids saliva, sweat and tear compared to biochemical hydration assessment markers within blood and urine.” European Journal of Clinical Nutrition. 2018;72(1):69–76. doi:10.1038/ejcn.2017.136
9. McKenzie AL, Muñoz CX, and Armstrong LE. “Accuracy of Urine Color to Detect Equal to or Greater Than 2% Body Mass Loss in Men.” Journal of Athletic Training. December 2015;50(12):1306–1309.
10. Armstrong LE, Maresh CM, Castellani JW, et al. “Urinary Indices of Hydration Status.” International Journal of Sport Nutrition. 1994;4(3):265–279.
11. Imran S, Eva G, Christopher S, Flynn E, and Henner D. “Is specific gravity a good estimate of urine osmolality?” Journal of Clinical Laboratory Analysis. 2010;24(6):426–430. doi: 10.1002/jcla.20424. PMID: 21089176; PMCID: PMC6647580.
12. Walawender L, Patterson J, Strouse R, et al. “Mobile Technology Application for Improved Urine Concentration Measurement Pilot Study.” Frontiers in Pediatrics. 2018 Jun 6;6:160. doi: 10.3389/fped.2018.00160. PMID: 29928640; PMCID: PMC5998741.





