
Injuries are an unfortunate part of sports and can be physically and emotionally taxing on an athlete. As such, optimizing one’s rehabilitative process for a full return to sport is of paramount importance for athletes and clinicians alike.
While appropriate physical training can reduce the risks associated with sustaining musculoskeletal injuries, they can never be entirely eliminated. Because of this, there will always be a need for recovery interventions that can augment and accelerate the athlete’s recovery back to pre-injury status (and hopefully beyond this level).
Of the multitude of therapeutic modalities and strengthening interventions that can be utilized for rehabilitating musculoskeletal injuries, one exciting intervention—blood flow restriction therapy (BFR)—has been gaining popularity over recent years, particularly for the lower extremities. The lower extremity is reported to be the most frequently injured area of the body, with the hamstrings and the rectus femoris (a quadriceps muscle) being two of the most commonly injured muscles of the lower extremity.1–3
The popularity of an intervention doesn’t necessarily guarantee its effectiveness, but a look at the scientific literature on blood flow restriction therapy backs up the claims. Share on XBut the popularity of an intervention doesn’t necessarily guarantee its effectiveness. So, if this therapeutic intervention is as effective as many claim it to be, a look at the scientific literature should back it up. And—spoiler alert—it does.
However, simply having a general awareness of an intervention’s effectiveness doesn’t mean much if you don’t understand the nature of when, how, and why it can be utilized.
So, let’s break this all down and let science lead the way!
Challenges with Lower Extremity Injuries
Regaining muscle strength and mass following injury is necessary for a successful return to sport. When injured, the longer the athlete goes without physically loading and stimulating the affected muscles (in this case, the muscles within their lower extremity), the greater the loss of strength and the greater the extent of muscle atrophy (shrinking) they will experience.4
The principle of progressive overload involves repeated stimulation of specific muscles (typically through a resistance training program) to induce favorable morphological changes in these targeted tissues. These changes can include the following:
- Structural changes to muscle fibers (increasing their contractile strength).
- Increasing the cross-sectional area (CSA) of muscle fibers.
- Improved neuromuscular efficiency between the neuromuscular junction.
With traditional strength training, an individual must use resistance of approximately 65%–70% of their one-repetition maximum (1RM) to trigger a stimulus that will elicit increases in muscle size (muscle hypertrophy) and strength.5,6
The problem for the injured athlete is the extent of required muscular force and effort needed to elicit these positive changes via progressive overload. The required 65%–70% maximal contractile ability can easily exceed the force production capabilities of the injured muscles and tendons (especially in earlier phases of injury recovery), which could lead to increased pain, further injury, and, ultimately, a prolonged recovery.
Additionally, the athlete may have otherwise healthy muscles but an injured or painful joint (hip, knee, ankle, etc.) incapable of bearing such loads. This inability to put such a load through a joint essentially determines how much stimulus its associated muscles can receive.
The longer the athlete must go without adequate muscle stimulus, the more extensive their loss of functional capacity will be within the limb. And herein lies the problem for many athletes and rehabilitative specialists: How do you make a muscle stronger when it (or its associated joint) doesn’t have the capacity to withstand the mechanical stress required for physical strengthening?
The traditional route taken by many rehabilitative specialists is the use of neuromuscular electrical stimulation (NMES), which involves placing electrodes over the targeted muscles and delivering an external electrical current through the skin, making the muscles contract.
While NMES certainly has a time and a place in musculoskeletal rehab, it also has its drawbacks, two of which are:
- The ability of the electrode pads to only target superficial muscles and not necessarily deeper muscles.7
- A highly inefficient and unnatural pattern of motor unit recruitment when compared to the body’s own motor unit recruitment pattern via the nervous system.8
Also, NMES cannot account for providing functional and sport-based movements that the athlete requires in late-stage rehab as part of a return-to-play protocol.
As such, a better way to provide adequate strength-inducing stimuli to injured muscle tissue has remained rather elusive for athletes and healthcare practitioners alike up until recently.
What Is Blood Flow Restriction Therapy?
Enter blood flow restriction therapy, a strength training intervention involving a restrictive cuff placed around the injured or affected limb with a predetermined amount of circumferential tension. This tension partly (but not fully) impedes blood flow to the working extremity and is maintained while the athlete or individual performs exercise against a predetermined load.
And here’s the kicker: That predetermined load doesn’t have to be anywhere near traditional strength training loads to elicit positive effects on the muscle(s).
Numerous studies have shown that BFR therapy can produce statistically significant changes in muscle size and strength when exercising at only 20%–30% of the individual’s 1RM rather than the traditional 65%–70% 1RM.9–12
Numerous studies have shown that BFR therapy can produce statistically significant changes in muscle size and strength when exercising at only 20%–30% of the individual’s 1RM. Share on XThis allows the athlete to initiate strength training interventions much earlier in their rehab, equating to significantly decreased mechanical stress on the injured (and still vulnerable) tissues and structures.
BFR has been studied in various demographics, ranging from young, healthy athletes to frail, injured, and elderly populations. As such, it also has a time and place outside the world of rehabilitation. For the sake of this article, however, I’ll only focus on rehabilitative interventions within active populations.
How Does BFR Work?
While the exact mechanisms of BFR’s abilities to positively impact muscle strength and size at such a low intensity aren’t fully understood, there exists a decent amount of scientific data suggesting that the factors most responsible for BFR’s positive effects include:
- Metabolic changes to the local muscle environment (state of hypoxia, enzymatic changes, lactate levels, etc.).
- Neuromuscular changes, such as altered motor unit firing and recruitment patterns.
- Endocrine (hormonal) changes, including plasma growth therapy hormone (GH), norepinephrine (NE), and insulin-like growth factor-1 (IGF-1).
Essentially, this means that low-load BFR training likely produces favorable changes in muscle size and strength through mechanisms other than strictly through mechanical tension alone.13,14
Traditional strength training relies extensively on muscle changes arising through mechanical tension. However, due to the low loads utilized with BFR, it seems that mechanical tension doesn’t play an extensive role when compared to the various metabolic changes it has shown to create within the targeted muscles. It is also possible that the combination of these two factors is responsible for the positive muscular effects seen with BFR training.
How to Perform BFR Training
BFR training for the lower extremities is most often performed by placing the restrictive cuff just below the gluteal fold of the thigh (just beneath your butt cheek). The cuff is placed as high as possible around the extremity to ensure that:
- The cuff does not impede movement or create discomfort when moving or exercising.
- The injured tissue is distal to (beneath) the area of cuff restriction.
- The greatest extent of metabolic buildup occurs by having as much muscle fiber as possible undergo the restricted rate of blood flow.

When it comes to using restrictive cuffs, two primary cuff types can be utilized:
- Elastic bands or wraps.
- Pneumatic cuffs.
Elastic bands are the least expensive and most readily available options for most athletes. These can include common fitness bands such as Voodoo flossing bands or powerlifting knee wraps. While inexpensive and easy to acquire, their main drawback is their lack of dedicated feedback to ensure ideal pressure around the limb is utilized.
Pneumatic (air pressure) cuffs are the second option. While they’re more expensive and less readily available, they provide the user with accurate pressure readings for how much pressure is being placed around the extremity. These cuffs work by increasing the pressure around the extremity through manually controlled or automatically controlled means. The complexity (and subsequent cost) of these cuffs can range significantly from one system to the next.

Cuff Width and Pressure
Selecting ideal restriction pressure should be of paramount interest when performing BFR therapy; too little pressure will nullify any benefits derived from BFR, while excessive pressure can lead to excessive discomfort, pain, and numbness and prevent successful completion of the exercise.
Many studies that have examined the strength and cross-sectional area enhancement of muscle tissue with BFR therapy utilize restriction pressures ranging from 140 mmHg to 240 mmHg. A pressure ranging between 160 mmHg and 180 mmHg is often used, as this amount of pressure will occlude femoral arterial blood flow by 50%.15
Cuff width can also play a factor in the overall comfort of BFR therapy. Cuffs wider than 13.5 centimeters have been shown to cause greater subjective amounts of pain than cuffs 5 centimeters wide and inflated to the same pressure (200 mmHg).16
Exercises, Sets, and Reps
Exercise parameters utilized for BFR training can vary significantly based on numerous factors pertaining to the injured athlete. This can include the location and severity of their muscular injury, the stage of rehab, current pain levels, and other factors unique to the athlete. As such, there is plenty of room for the clinician to draw from their clinical expertise when employing BFR therapy.
Generally speaking, lower extremity exercises involving large and multiple muscle groups are ideal. The scientific literature commonly features studies using leg extensions. However, numerous other exercises can be utilized based on the athlete’s needs and equipment availability.

While there is no universal “right or wrong” protocol to follow when performing strengthening exercises, a highly utilized set and rep scheme within the scientific literature is the 30/15/15/15 protocol, which has been shown to be effective.17–20
This protocol involves performing the initial exercise set for 30 repetitions, followed by a 30-second break. From there, 15 repetitions are performed for the second set, with a 30-second break afterward. This process is repeated until four total sets have been completed, with the last three sets consisting of 15 repetitions each.
The first set involves a higher repetition scheme with the belief that it will foster a more extensive metabolic change within the working and surrounding muscles. The short breaks between sets help ensure that the working muscles receive an inadequate recovery, helping to continually change the metabolic environment within the muscles.
Results of BFR therapy are best obtained by utilizing a continuous pressure (i.e., keeping the limb partially occluded during rest breaks) rather than an intermittent pressure. Share on XIt’s important to mention that results of BFR therapy are best obtained by utilizing a continuous pressure (i.e., keeping the limb partially occluded during rest breaks) rather than an intermittent pressure (where pressure is relieved between sets).21

For athletes in the early stages of rehab, or those not accustomed to BRF interventions, one singular exercise may be ideal. As the athlete gains confidence, strength, and endurance, additional exercises can likely be added. As a general rule, maximal cuff time should not exceed 20 minutes.
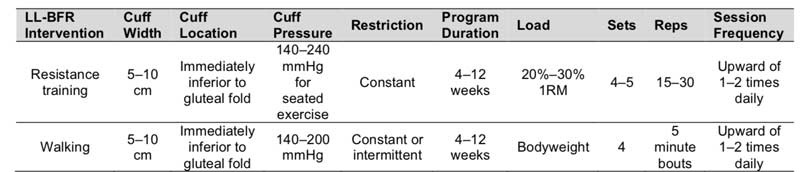
Additionally, it’s worth noting that BFR interventions can also involve walking protocols. Walking protocols have been commonly studied and produce favorable outcomes in muscle strength and hypertrophy.22–24 While these protocols aren’t covered within this article, I have included general parameters in table 1.
How Often Should You Perform BFR Training?
With traditional strength training, the amount of mechanical stress the working muscles undergo necessitates a recovery period of anywhere from 48–72 hours before the muscles can tolerate another strength training stimulus.
With BFR therapy, this recovery period is typically not required, as the low 20%–30% intensity places minimal mechanical stress on the muscles and tendons compared to traditional strength training at higher loads. It is also much less taxing on the central nervous system.
Numerous scientific studies have implemented BFR training protocols ranging from twice a week to twice a day. While the training frequency most ideal for the injured athlete will be dictated by numerous factors (type of injury, stage of recovery, lifestyle factors, etc.), generally speaking, BFR therapy can take place at a much greater weekly frequency than with traditional strength training.25,26 This high volume of frequent, low-intensity stimulations can likely greatly assist with the rate of recovery.
Generally speaking, BFR therapy can take place at a much greater weekly frequency than therapy with traditional strength training. Share on XIn general, a higher frequency of BFR intervention has yielded more favorable results than a lower session frequency, so long as exercise repetitions are not taken to volitional exhaustion (doing so can lead to delayed onset muscle soreness, which leads to reduced training frequency).
Safety Considerations with BFR Training
The most effective therapy in the world doesn’t mean much if it isn’t safe. As such, understanding the general consensus on the safety of BFR therapy (and its contraindications) is vital to anyone utilizing this intervention.
On the whole, BFR therapy is regarded to be a safe intervention for otherwise healthy populations, based on multiple studies examining various safety aspects.
On the whole, BFR therapy is regarded to be a safe intervention for otherwise healthy populations, based on multiple studies examining various safety aspects. Share on XSome of these aspects include:27,28
- No impact on blood clotting when examined by changes in fibrin D-dimer.
- No impact on peripheral vascular mechanics.
- No impact on peripheral nerve conduction.
When Not to Use BFR Therapy (Contraindications)
As with any other therapeutic modality or intervention, there are times when BFR shouldn’t be utilized. While not an exhaustive list, general contraindications include the following:29
- History of deep venous thrombosis (blood clots).
- Varicose veins.
- Pregnancy.
- Over open wounds or skin lesions.
- Diminished, absent, or altered sensation within the lower extremity.
Best Bet for Motivated Athletes
Every rehabilitative intervention has a time and place for its use. With BFR therapy, the best results will likely be obtained with motivated athletes who wish to take an active role in their rehabilitation. By appropriately stimulating (and challenging) skeletal muscle fiber at earlier phases of injury recovery, the athlete is likely to minimize muscle atrophy and strength loss while subsequently reducing time spent on the sidelines.
Since you’re here…
…we have a small favor to ask. More people are reading SimpliFaster than ever, and each week we bring you compelling content from coaches, sport scientists, and physiotherapists who are devoted to building better athletes. Please take a moment to share the articles on social media, engage the authors with questions and comments below, and link to articles when appropriate if you have a blog or participate on forums of related topics. — SF
References
- Briggs AM, Cross MJ, Hoy DG, et al. “Musculoskeletal health conditions represent a global threat to healthy aging: A report for the 2015 World Health Organization world report on ageing and health.” The Gerontologist. 2016;56(suppl_2):S243–S255.
- Kell RT, Bell G, and Quinney A. “Musculoskeletal fitness, health outcomes and quality of life.” Sports Medicine. 2001;31(12):863–873.
- Chan O, Del Buono A, Best TM, and Maffulli N. “Acute muscle strain injuries: A proposed new classification system.” Knee Surgery, Sports Traumatology, Arthroscopy. 2012;20(11):2356–2362.
- Hart JM, Pietrosimone B, Hertel J, and Ingersoll DC. “Quadriceps Activation Following Knee Injuries: A Systematic Review.” Journal of Athletic Training. 2010;45(1):87–97. doi:10.4085/1062-6050-45.1.87
- Wernbom M, Augustsson J, and Roland T. “The Influence of Frequency, Intensity, Volume and Mode of Strength Training on Whole Muscle Cross-Sectional Area in Humans.” Sports Medicine. 2007;37(3):225–264. doi:10.2165/00007256-200737030-00004
- Schoenfeld BJ. “The Mechanisms of Muscle Hypertrophy and Their Application to Resistance Training.” Journal of Strength and Conditioning Research. 2010;24(10:2857–2872. doi:10.1519/JSC.0b013e3181e840f3
- Fuglevand AJ, Winter DA, Patla AE, and Stashuk D. “Detection of motor unit action potentials with surface electrodes: influence of electrode size and spacing.” Biological Cybernetics. 1992;67(2):143–153.
- Doucet BM, Lam A, and Griffin L. “Neuromuscular electrical stimulation for skeletal muscle function.” Yale Journal of Biology and Medicine. 2012;85(2);201.
- Loenneke JP, Wilson JM, Marín PJ, Zourdos MC, and Bemben MG. “Low intensity blood flow restriction training: a meta-analysis.” European Journal of Applied Physiology. 2012:112(5):1849–1959. doi:10.1007/s00421-011-2167-x
- Slysz J, Stultz J, and Burr JF. “The efficacy of blood flow restricted exercise: A systematic review & meta-analysis.” Journal of Science and Medicine in Sport. 2016;19(8):669–675. doi:10.1016/j.jsams.2015.09.005
- Hughes L, Paton B, Rosenblatt B, Gissane C, and Patterson SD. “Blood flow restriction training in clinical musculoskeletal rehabilitation: a systematic review and meta-analysis.” British Journal of Sports Medicine. 2017;51(13):1003–1011. doi:10.1136/bjsports-2016-097071
- Centner C, Wiegel P, Gollhofer A, and König D. “Effects of blood flow restriction training on muscular strength and hypertrophy in older individuals: a systematic review and meta-analysis.” Sports Medicine. 2019;49(1):95–108.
- Pearson SJ and Hussain SR. “A Review on the Mechanisms of Blood-Flow Restriction Resistance Training-Induced Muscle Hypertrophy.” Sports Medicine. 2015;45(2):187–200. doi:10.1007/s40279-014-0264-9
- Loenneke JP, Wilson GJ, and Wilson JM. “A Mechanistic Approach to Blood Flow Occlusion.” International Journal of Sports Medicine. 2010;31(1):1–4. doi:10.1055/s-0029-1239499
- Takano H, Morita T, Iida H, et al. “Hemodynamic and hormonal responses to a short-term low-intensity resistance exercise with the reduction of muscle blood flow.” European Journal of Applied Physiology. 2005;95(1):65–73. doi:10.1007/s00421-005-1389-1
- Rossow LM, Fahs CA, Loenneke JP, et al. “Cardiovascular and perceptual responses to blood-flow-restricted resistance exercise with differing restrictive cuffs.” Clinical Physiology and Functional Imaging. 2012;32(5):331–337.
- Martín-Hernández J, Marín PJ, Menéndez H, Ferrero C, Loenneke JP, and Herrero AJ. “Muscular adaptations after two different volumes of blood flow-restricted training: Analysis of occlusion training volume.” Scandinavian Journal of Medicine & Science in Sports. 2013;23(2):e114–e120.
- Yasuda T, Ogasawara R, Sakamaki M, Ozaki H, Sato Y, and Abe T. “Combined effects of low-intensity blood flow restriction training and high-intensity resistance training on muscle strength and size. European Journal of Applied Physiology. 2011;111(10):2525–2533. doi:10.1007/s00421-011-1873-8
- Vechin FC, Libardi CA, Conceição MS, et al. “Comparisons Between Low-Intensity Resistance Training With Blood Flow Restriction and High-Intensity Resistance Training on Quadriceps Muscle Mass and Strength in Elderly.” The Journal of Strength and Conditioning Research. 2015;29(4):1071–1076. doi:10.1519/JSC.0000000000000703
- Yasuda T, Loenneke JP, Thiebaud RS, and Abe T. “Effects of Blood Flow Restricted Low-Intensity Concentric or Eccentric Training on Muscle Size and Strength.” Garatachea N, ed. PloS ONE. 2012;7(12):e52843. doi:10.1371/journal.pone.0052843
- Fahs CA, Loenneke JP, Rossow LM, Tiebaud RS, and Bemben MG. “Methodological considerations for blood flow restricted resistance exercise.” Journal of Trainology. 2012;1(1):14–22. doi:10.17338/trainology.1.1_14
- Sakamaki M, Bemben MG, and Abe T. “Legs and trunk muscle hypertrophy following walk training with restricted leg muscle blood flow.” Journal of Sports Science and Medicine. 10(2):338.
- Abe T, Kearns CF, and Sato Y. “Muscle size and strength are increased following walk training with restricted venous blood flow from the leg muscle, Kaatsu-walk training.” Journal of Applied Physiology. 2006;100:7.
- Abe T, Kearns CF, Fujita S, Sakamaki M, Sato Y, and Brechue WF. “Skeletal muscle size and strength are increased following walk training with restricted leg muscle blood flow: implications for training duration and frequency.” International Journal of KAATSU Training Research. 2009;5(1):9–15. doi:10.3806;ijktr.5.9
- Fujkita T, Brechue WF, Kurita K, Sato Y, and Abe T. “Increased muscle volume and strength following six days of low-intensity resistance training with restricted muscle blood flow.” International Journal of KAATSU Training Research. 2008;4(1):1–8.
- Abe T, Yasuda T, Midorikawa T, et al. “Skeletal muscle size and circulating IGF-1 are increased after two weeks of twice daily “KAATSU” resistance training.” International Journal of KAATSU Training Research. 2005:1(1):6–12. doi:10.3806/ijktr.1.6
- Clark BC, Manini TM, Hoffman RL, et al. “Relative safety of 4 weeks of blood flow-restricted resistance exercise in young, healthy adults: Blood flow restricted exercise.” Scandinavian Journal of Medicine & Science in Sports. 2011;21(5):543–662. doi: 10.111/j.1600-0838.2010.01100.x
- Loenneke JP, Wilson JM, Wilson GJ, Pujol TJ, and Bemben MG. “Potential safety issues with blood flow restriction training: Safety of blood flow-restricted exercise.” Scandinavian Journal of Medicine & Science in Sports. 2011;21(4):510–518. Doi:10.1111/j.1600-0838.2010.01290.x
- Mason MJS, Owens JG, and Brown LWJ. “Blood flow restriction training: Current and future applications for the rehabilitation of musculoskeletal injuries. Techniques in Orthopaedics. 2018;33(2):71.

