Since the country’s infection and identification of the COVID-19 virus, several distinct restrictions and recommendations have been placed on the public in an attempt to control the spread of this disease. For athletics, these constraints have raised concerns for the sustained performance enhancement training of athletes and the future anticipation for the return of organized sports at the high school, collegiate, and professional levels of competition. Numerous news reports, internet blogs, ZOOM meetings, and podcasts have conveyed concern about the return to play (RTP) of “healthy” athletes who have had to modify, at best, their required training due to the COVID-19 pandemic. A noteworthy unknown is how athletes will fair physically at the time of the approval and initiation of formal, organized sport team practice sessions and eventual game day competition.
A training topic that has not had as much deliberation is the effect of the COVID-19 restrictions upon the injured and post-surgical athlete’s rehabilitation and their level of physical condition when they also return to sport team practice. As the pandemic has resulted in many athletes returning to their homes, the present circumstances have affected the athlete’s capability to continue with appropriate and effective rehabilitative care. Although physical therapy is classified as an essential business of the health care continuum, many private outpatient health care facilities, as with other various businesses, have either closed or suspended their operations. The restrictions in accessibility raise additional concerns of how the injured or postoperative athlete will fair in their physical preparedness for daily sport team practice and game day competition.
How will injured or postoperative athletes fair in their physical preparedness for team practice & game day when COVID restrictions lift? Share on XCompetitive athletics transpire in a physical and, at times, hostile environment. It’s a setting where many unfortunate sport injuries, some requiring surgical intervention, may plague an athlete for an extended time. Once they complete their sports rehabilitation, they’re required to participate in a battery of tests to assess their physical prowess for a possible return to sport participation. The content of this post emphasizes our alternative perspective for the athlete’s post-rehabilitation RTP testing, and more specifically, the RTP testing of the anterior cruciate ligament (ACL) injured and ACL reconstructed (ACLR) knee athlete. We’ve used this RTP testing program successfully and progressively modified it periodically over the past few years for the athlete’s safe and optimal return to athletic competition.
Present-day athletes are stronger, more powerful, and faster than the athletes of decades past. Training philosophies, programming, equipment, nutrition, sports science, and sports medicine services and techniques have evolved specifically to enhance the physical standards of athletic performance. Unfortunately, participation in athletic competition comes with the potential for athletic injuries. Sports medicine professionals and scientists have investigated the cause and effect of numerous sport injuries over the past decades in an attempt to improve both the prevention (reduction) and care of these injuries. One highlight has been the efforts to improve the surgical intervention, rehabilitation, and RTP testing of the ACL injured and ACLR knee athlete.
The RTP outcomes of these athletes during the COVID-19 pandemic remain relatively unknown due to the unfamiliarity of the current circumstances. The environment that confines the athlete’s ability to train compounded by the uncertainty for appropriate sports rehabilitative care makes for a valid concern for the athlete’s RTP outcomes. Also, some individuals may have some degree of hesitation for attending “face-to-face” rehabilitation sessions due to the pandemic.
Before the COVID-19 pandemic, there were more than 300,000 ACL reconstructions performed in the United States annually, according to reports. Of these, 20% to 50% will not return to the same sport they participated in after surgery, and 10% to 70% of those who return will do so at a substandard performance level.1, 2 Investigators who performed an in-depth meta-analysis on this subject found only a 47% return to previous levels of sport participation several years after primary ACLR.3
RTP ACLR athletes often have deficits in the physical qualities required for optimal athletic performance, leaving them at risk for a later ACL injury. Share on XUnfortunately, the RTP ACLR athlete often presents with deficits in the physical qualities required for optimal athletic performance, leaving them at risk for a later ACL injury.4, 5Subsequent ACL injuries approach 49%,6 suggesting there are shortcomings in the current RTP ACLR testing criteria. Due to the COVID-19 alterations and limitations commenced in recent months, one may inquire whether the ACLR RTP outcomes will remain as reported or worsen when sport team practice and game day competition start.
Younger athletes (less than 20 years of age) who experience a second ACL injury also had lower “psychological readiness” 12 months after ACLR.7 This reduced psychological readiness is termed kinesiophobia, which may not be familiar to many strength and conditioning (S&C) and sport coaches. Kinesiophobia is an additional limiting factor in an athlete’s ability to return to optimal levels of athletic performance safely. Kinesiophobia is the fear of inducing pain or re-injury to the injured or postoperative anatomy and, explicitly for this discussion, the ACLR extremity. It results in a compromised physical performance that we may observe during physical rehabilitation, athletic performance enhancement training, team practice sessions, and game day competition. The fear of re-injury diminishes the athlete’s confidence and ability to distribute and receive substantial forces that are necessary for ideal levels of athletic performance. The kinesiophobia phenomenon in association with the physical deficits that may exhibit during ACLR RTP testing will result in a poor test score and prohibit the athlete’s return to sport.
Due to the causes previously noted, at the time of RTP testing, the ACLR athlete may present with a lack of strength. Strength is important for both force application and absorption, muscle and joint stiffness, joint stability, and injury prevention (reduction) and is the physical quality from where all other physical qualities evolve. The lack of ideal strength levels places the athlete at athletic performance and RTP testing disadvantage.
A deficiency in relative strength values may result in muscle and mechanical damage8 as well as decreased performance in sprinting, jumping, deceleration, and change of direction.9Weaker athletes also tend to rely more on their ligaments for joint stability in high-intensity situations, a phenomenon known as ligament dominance.10 Ligament dominance places the athlete at risk of re-injury by emphasizing knee joint stability upon the joint ligament structures, including the injured or reconstructed ACL as an alternative to the supporting knee joint musculature. Also, collegiate male and female athletes lacking relative back squat strength values of 2.2 and 1.6, respectively, may be susceptible to lower extremity injury throughout a sport season.11 Strength is a physical quality we should not undervalue.
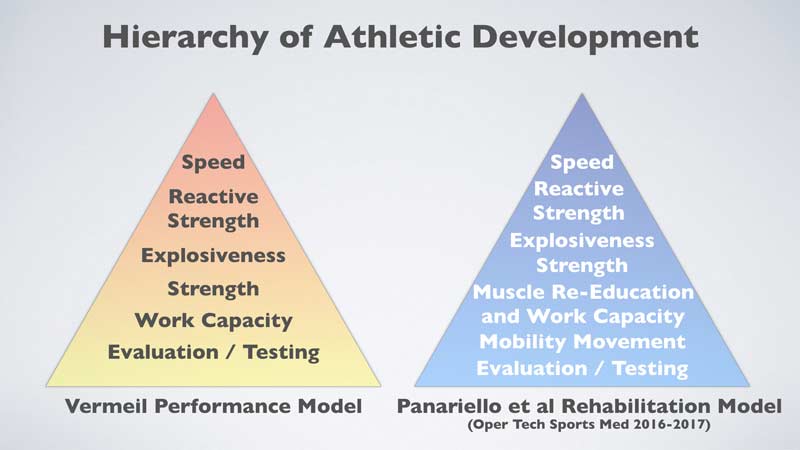
Our program design for the performance enhancement training and sports rehabilitation of our athletes is founded upon Hall of Fame (HOF) S&C coach Al Vermeil’s Hierarchy of Athletic Development (see Image 1). For many reasons confirmed in scientific literature, including noted published statements regarding the “shortcoming in the current RTP ACLR testing criteria,” we modified and adapted this hierarchy model for our ACL injury and ACLR RTP testing.12, 13
Traditional ACLR Return-to-Play Testing
Traditional ACLR RTP testing commonly involves a limb symmetry index (LSI) strategy, where the athlete’s documented RTP test scores of the ACLR lower extremity are compared to those of the non-involved (non-surgical) lower extremity. The RTP test score is expressed as a percentage of the non-surgical limb test scores, i.e., 90%, 95%, etc. The athlete’s RTP “clearance” is based on achieving a test score that meets or exceeds the standards established by the physician and rehabilitation team. Activities commonly prescribed in the RTP testing model include, but are not limited, to:
- Manual ACL ligament integrity testing
- Knee ligament arthrometer testing (if available)
- Isokinetic testing (if available)
- Neuromuscular testing
- Various bilateral and single-leg strength tests
- Various bilateral and single-leg jump tests
- Various bilateral and single-leg hop tests
- Various running and change of direction (COD) tests
- Various agility tests
A concern with the LSI test strategy is that the non-involved extremity has also experienced a period of deconditioning from the time of ACL injury, surgery, and the initial periods of rehabilitation. Also, the required postoperative “healing continuum” of soft tissue and bone results in medically prescribed limitations in the athlete’s level of physical activity over an extended period. These physical activity limitations not only result in deficits of the physical qualities in the ACLR extremity but also the non-involved extremity.14 The addition of COVID-19 precautions and environmental (training and rehabilitation) restrictions likely compound the deconditioning of both lower extremities as well as the athlete’s overall physical deconditioning. Therefore, the question arises whether we should consider the non-operative extremity the sole physical “gold standard” when deciding the athlete’s safe and optimal RTP.
LSI scores frequently overestimate knee function after ACLR and may be related to a subsequent risk for ACL injury. Share on XWellsandt15 reviewed 70 ACLR athletes for LSIs compared to their estimated pre-injury capacity (EPIC), meaning the non-involved lower extremity estimated physical qualities before the ACL injury. Of the 70 athletes, 40 (57.1%) achieved a 90% LSI score, while only 20 athletes (28.6%) met a 90% EPIC score. Twenty-four athletes (34.3%) who obtained a 90% LSI score did not achieve a 90% EPIC score. The authors concluded that LSI scores frequently overestimate knee function after ACLR and may be related to a subsequent risk for ACL injury.
The Physical Quality Standards of Sport
Although LSIs have been recognized as a method to help determine the athlete’s physical ability for RTP, our opinion is that they are only part of the equation. There are required physical quality standards associated with optimal athletic performance, which include the specific sport as well as the position played or event. If this was not true, why do professional sport combines exist to help determine not only the draft selection but also the round of each selection? Why are there running distance and sprinting times, throwing distance, and jumping distance and height qualifications for track and field events? Why are there total weight achievement performance qualifications for weightlifting events?
We should not disregard the physical standards of sport. As an example, let’s review the RTP of a major league baseball (MLB) pitcher who sustained a throwing arm injury (and possible surgery).
At the time of their progressive rehabilitation throwing program, the basic throwing sequence would likely be similar to the following:
- Short toss
- Long toss
- Pitching from flat ground
- Pitching from a pitcher’s mound (with mound height progressions)
These types of throwing programs produce outcomes that are not limited to improvement in arm strength, enhanced arm velocity, improvement in the neuromuscular timing of the shoulder complex, and total body unit as well as enhanced pitching mechanics. All are essential for the throwing athlete’s optimal RTP. However, if the athlete’s most effective pitch is a fastball, and the MLB standard for fastball velocity is 90-90+ miles per hour (mph), wouldn’t the athlete need to attain this pitching velocity standard for their RTP performance to be effective? If the rehabilitated MLB pitcher demonstrates a top RTP fastball velocity of 80 mph, they likely would not be assigned to pitch in an MLB game. Thus, if MLB has a position (pitcher) and physical standard (velocity) for that position, why would it be any different for any physical quality necessary for success in any sport, position, or event? Why would this RTP perspective be any different for any other various injured athlete anatomy?
The performance enhancement training, nutrition, and sports science of athletes are evolving to result in stronger, more powerful, and faster athletes. These advancements also result in the proverbial “raising of the bar” concerning the physical qualities and performance standards of sport. Acknowledging these innovations and physical quality enhancements, why would the RTP standard for the ACLR athlete be limited to an LSI comparison of the non-involved extremity? Why would the RTP testing not include the physical quality standards of the sport, position, or event in addition to the athlete’s LSI?
LSI test scores don't ensure that an ACL reconstructed athlete exhibits the physical quality standards necessary for their sport. Share on XThe LSI test scores do not ensure that the ACLR athlete exhibits the physical quality standards necessary for their particular sport. Our rationale for incorporating these standards as part of our RTP testing initiative is this: these physical standards are presented daily by the athlete’s peers during sport practice sessions and by the athlete’s opponent(s) on the high-intensity day of competition. Image 2 provides an example of the physical quality standards for college and high school football athletes.
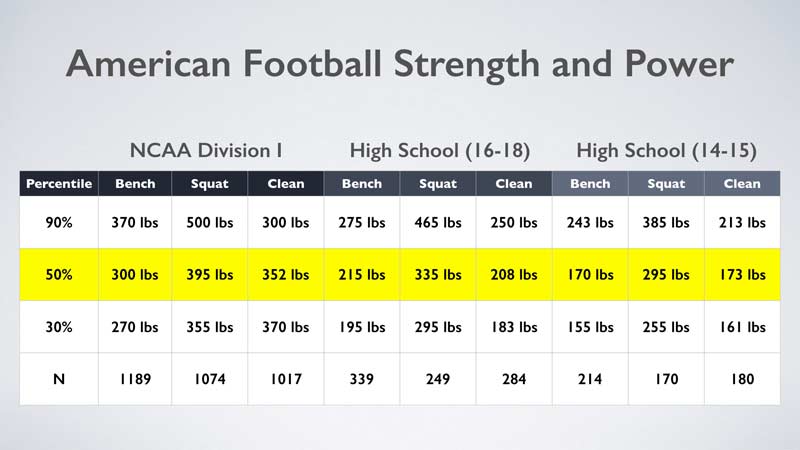
Reviewing Image 2, if a returning Division I football ACLR athlete demonstrates an LSI of 90% or greater yet executes a squat of 300 pounds, they would qualify below the 30thpercentile for the squat exercise performance. With their football peers demonstrating significant strength advantages (i.e., the 90th percentile equates to a 500-pound squat), would this not place the ACLR athlete at a disadvantage regarding their on-the-field performance, as well as a possible increased risk of acute injury or ACLR re-injury?
The RTP testing may also expose additional deficiencies of the remaining physical qualities in Vermeil’s hierarchy as related to the standards of sport. Therefore, in our opinion, LSI testing alone does not disclose a complete representation of the athlete’s potential on-the-field performance or potential risk of acute or ACLR re-injury.
ACL Injury and ACLR Return-to-Play Testing
As each physical quality in coach Vermeil’s hierarchy depends on the optimal development of its physical quality predecessor, enhancing each quality begins with strength. This is not to imply that we can’t address each quality simultaneously. However, we should emphasize the physical quality presenting with the greatest deficit, depending upon the athlete’s needs, in their performance enhancement training and rehabilitation. In our ongoing ACLR RTP study with over 300 high school and college athletes to date, we’ve found that RTP success depends not only on their time from surgery, as documented in the scientific literature, but also restoring their physical qualities based on the standards of sport for a safe return to optimal athletic performance.
Presently, the two most significant physical findings observed in our RTP testing are (1) deficits in the physical quality of strength, and (2) poor reactivity to the ground surface area, meaning propulsion, deceleration, and COD in vertical and deviating linear directions. We’re not insinuating that additional physical deficiencies are not exposed; however, due to these particular physical deficiencies, compensatory body postures are noted during the testing.The inability to apply appropriate levels of force as well as tolerate ground reaction forces result in extended time spent on the ground. This extended time places consequences on the overall RTP testing performance. Compensatory adjustments in body postures also put excessive and unaccustomed stresses on various anatomical structures. As these repetitive stresses accumulate over time, they may set the stage for possible acute injury or future ACLR re-injury. It’s also important to note that, when the discrepancy in strength is resolved, other physical qualities, ground reaction times, and body postures frequently improve as well.
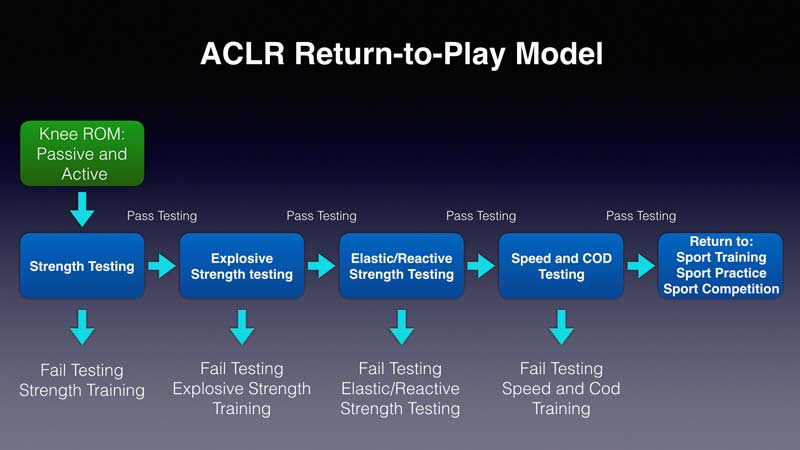
Our RTP model, as in other reported post-rehabilitation lower extremity RTP testing, includes a variety of tests to assist in determining the athlete’s safe and ideal return to sport. Image 3 depicts the specific components of our RTP testing, as influenced by Vermeil’s hierarchy, where our experiences differ from “traditional” ACLR RTP testing.12
Active Knee Range of Motion
One of the immediate objectives during rehabilitation is to address knee range of motion (ROM) and, more specifically, active knee range of motion (AROM). After ACLR surgery, an urgent priority is to achieve full active knee extension as soon as possible. Full AROM knee extension is imperative during the normal ambulatory gait cycle, as full knee extension is the required joint position at heel strike. A lack of full knee extension will exacerbate the ACLR knee condition via the repetitive and accumulative joint stresses of each heel strike upon a flexed knee.
Comparatively, full AROM knee flexion is not usually stressed very early in the rehabilitation process. The emphasis placed on initial knee flexion is typically passive (PROM). PROM knee flexion can be attained safely and progressively over an appropriately prescribed time period. Full PROM knee flexion establishes the soft tissue compliance necessary to eventually achieve the active and efficient backside mechanics required for optimal running velocities.
At the ACLR RTP testing, we evaluate the athlete’s knee AROM before assessing their physical qualities. We’ve observed that full AROM is usually achieved for the athlete’s knee extension abilities but does not typically transpire for knee flexion. Full active knee flexion is required to attain an appropriate foot placement at the gluteal fold during the backside mechanics of the running gait cycle (see Image 4). Achieving the athlete’s AROM knee flexion during the rehabilitation process was a lesson presented to me over 30 years ago by my good friend Dr. Donald Chu. As running is a cyclical activity, poor backside mechanics will likely result in poor front side mechanics, and a poor single-leg running cycle will result in a poor overall running cycle.
AROM activities such as butt kicks and Mach series running drills prescribed in a safe and appropriate progression are two of the various activities that help achieve the desired active knee flexion. This active knee motion is significant and is a requirement for the athlete to return to their pre-injury efficient running velocities. Attaining full active knee flexion during rehabilitation will avoid the time necessary to accomplish this task when the athlete returns to athletic performance training.
Achieving full active knee flexion during rehab avoids taking time to accomplish this task when the athlete returns to athletic performance training. Share on X
ACLR RTP Testing of the Physical Qualities for Athletic Performance
At the time of the athlete’s ACLR RTP testing, we acknowledge the advantageous contribution of genetics in both the healing continuum as well as the athlete’s ability to execute optimally during RTP testing. We also recognize there are physical qualities that need to be reestablished for the athlete to RTP safely and allow for optimal athletic performance. When testing for a particular physical quality, it’s important to select an activity that appropriately measures the quality without any ensuing consequences from incompetent exercise execution. For example, consider the squat exercise designated as a strength test. If the athlete has never performed or is incapable of doing a technically proficient squat exercise, the consequences of a poorly executed squat will contribute to lower test score vs. a pure deficiency in strength qualities. Circumstances may arise, therefore, where an alternative exercise requiring less technical proficiency may be more suited for an athlete’s strength or other physical quality testing. During the testing process, it’s important to distinguish between the deficiencies in technical skill performance vs. an actual deficiency in the particular physical quality.
In our ACLR RTP algorithm (see Image 3), we assess each physical quality in the order depicted in coach Vermeil’s hierarchy. Strength is the first physical quality, and if the athlete passes the strength testing, they continue to the next quality of explosive strength. If the athlete passes this test, they test their elastic/reactive strength qualities, and so on. If the athlete fails a particular category, the testing stops, and they receive a training program designed to enhance the quality that failed. Once they complete the training program, the athlete returns for their scheduled retesting.
We don’t find it beneficial to continue an athlete’s ACLR RTP testing once they fail a physical quality category. In our experience, if an athlete fails a particular physical quality, they will likely perform poorly in the next physical quality test(s) in the hierarchy. For example, because strength is defined as the ability to produce force—and explosive strength incorporates a velocity component for force production—if an athlete is unable to produce adequate levels of applied force, how could they possibly exert adequate levels of applied force rapidly? When the athlete passes the entire ACLR RTP examination, we decide whether they should return to performance enhancement training, team practice, or sport competition. To make this decision, we have a collaborative discussion among the physician, rehabilitation team, S&C staff, and sport coaches.
Summary
The ACLR RTP testing is an integral component of our post-injury and post-surgical ACL knee rehabilitation program. Customary ACLR RTP testing uses LSIs to compare the involved lower extremity to the non-involved lower extremity, which is recorded as a percentage. In our opinion, LSI testing does not encompass the entire ACLR RTP criteria. This is especially a concern with the current training and rehabilitation constraints placed on athletes during the COVID-19 pandemic. Assessing specific physical qualities necessary for optimal athletic performance should be a consideration for the athlete’s ACLR RTP testing. And we should interpret these test results based on the physical standards of the athlete’s sport of participation as well as their particular position or sport event. Restoring the athlete’s physical qualities to equal the physical standards of sport will also instill confidence in their ability to apply and accept the forces placed upon them and their ACLR extremity in various athletic settings (i.e., team training, team practice, team competition). It also will help reduce, if not disregard, concerns of kinesiophobia. When we discount the physical standards recognized and exhibited by both the athlete’s peers during daily team sport practice and their opponents during the high-intensity game day competition, we may place the ACLR athlete at a physical disadvantage for athletic performance and present a possible risk for additional acute injury or ACLR re-injury.
Since you’re here…
…we have a small favor to ask. More people are reading SimpliFaster than ever, and each week we bring you compelling content from coaches, sport scientists, and physiotherapists who are devoted to building better athletes. Please take a moment to share the articles on social media, engage the authors with questions and comments below, and link to articles when appropriate if you have a blog or participate on forums of related topics. — SF
References
1. Kvist J, Ek A, Sporrstedt K, Good L, “Fear of Re-Injury: A Hindrance for Returning to Sports After Anterior Cruciate Ligament Reconstruction,” Knee Surg Sports Traumatol Arthrosc, 2005; 13(5): 393-397.
2. Chmielewski, TL, et al., “The Association of Pain and Fear of Movement/Reinjury with Function During Anterior Cruciate Ligament Reconstruction Rehabilitation,” J Orthop Sports Phys Ther, 2008; 38(12): 746-753.
3. Arden CL, et al., “Return to Sport Following Anterior Cruciate Ligament Reconstruction Surgery: A Systematic Review and Meta-Analysis of the State Of Play,” Br J Sports Med, 2011; 45(7): 596-606.
4. Hunnicutt JL, et al., “Quadriceps Neuromuscular and Physical Function After Anterior Cruciate Ligament Reconstruction.” J Athl Train, 2020; 55(3): 238-245.
5. Webster KE, Feller JA, “A Research Update on the State of Play for Return After Anterior Cruciate Ligament Reconstruction,” J Orthop Traumatol, 2019; 20(1):10.
6. Read PJ, et al., “Lower Limb Kinetic Asymmetries in Professional Soccer Players With and Without Anterior Cruciate Ligament Reconstruction: Nine Months Is Not Enough Time to Restore ‘Functional’ Symmetry or Return to Performance,” Am J Sports Med, 2020; 48(6): 1365-1373.
7. McPherson AL, et al., “Psychological Readiness to Return to Sport Is Associated With Second Anterior Cruciate Ligament Injuries,” Am J Sports Med, 2019; 47(4): 857-862.
8. Newton M, et al., “Comparison of Responses to Strenuous Eccentric Exercise of the Elbow Flexors Between Resistance-Trained and Untrained Men,” Journal of Strength and Conditioning Research, 2008; 22(2): 597-607.
9. Watts D, “A Brief Review on the Role of Maximal Strength in Change of Direction Speed,”J Aust Strength Cond, 2015; 23(2): 100-108.
10. Hewitt T, et al., “Understanding and Preventing ACL Injuries: Current Biomechanical and Epidemiologic Considerations–Update,” North American Journal of Sports Physical Therapy, 2010; 5(4): 234-251.
11. Case M, Knudson DV, Downey DL, “Barbell Squat Relative Strength as an Identifier for Lower Extremity Injury in Collegiate Athletes,” Journal of Strength and Conditioning Research, 2020; 34(5): 1249-1253.
12. Panariello, RA, Stump TJ, and Maddalone D, “Postoperative Rehabilitation and Return to Play after Anterior Cruciate Ligament Reconstruction,” Operative Techniques in Sports Medicine, 2016; 24(1): 35-44.
13. Panariello, RA, et al., “The Lower Extremity Athlete: Post-Rehabilitation Performance and Injury Prevention Training,” Operative Techniques in Sports Medicine, 2017; 25(3): 231-240.
14. Webster KE, Hewett TE, “Return-to-sport Testing Following ACL Reconstruction Revisited,” Brit J Sports Med, 2020; 54(1): 2-3.
15. Wellsandt E, Failla MJ, Snyder-Mackler, L, “Limb Symmetry Indexes Can Overestimate Knee Function After Anterior Cruciate Ligament Injury,” J Orthop Sport Phys Ther, 2017; 47(5): 334-338.
16. Hoffman J, Norms for Fitness, Performance, and Health, Human Kinetics, Champaign, IL, 2006.





