Dr. Martino Franchi is a post-doctoral Research Fellow at the MRC-ARUK Centre for Musculoskeletal Ageing, University of Nottingham, U.K. His main interest is to investigate, with an integrative physiology approach, the morphological, architectural, functional, and molecular mechanisms of skeletal muscle remodelling in response to different mechanical stimuli (mainly eccentric vs. concentric actions). Dr. Franchi’s research is ultimately focused on investigating the impact of aging on skeletal muscle features and the role of different exercise interventions in the preservation of muscle mass and quality as we age.
Freelap USA: Could you go into how scientists use sonography to look at muscle architecture? And what is the current consensus about adaptations to specific training regimes?
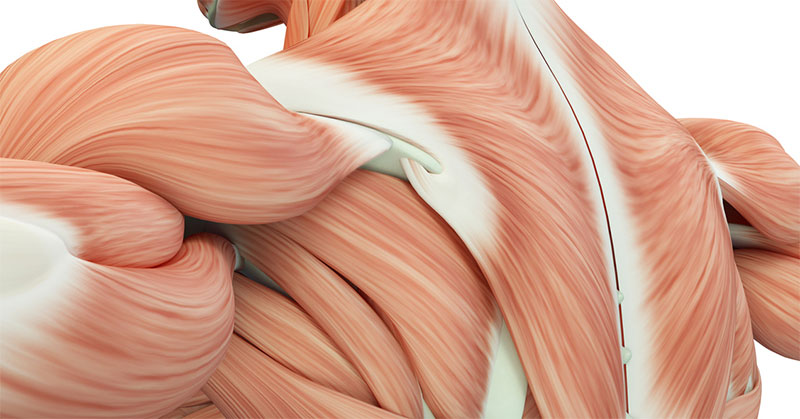
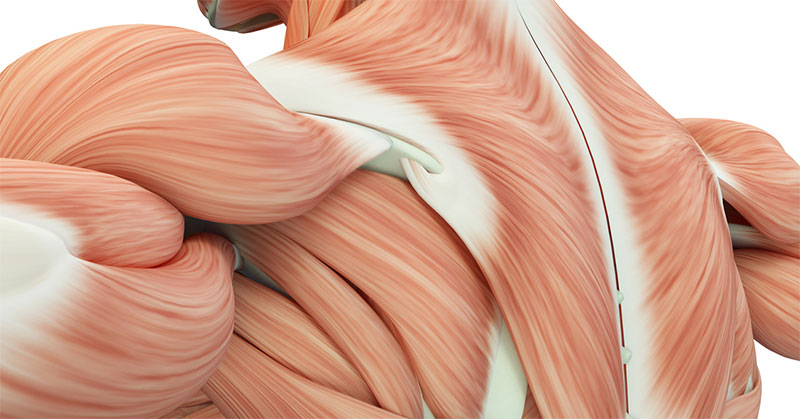
Martino Franchi: From scientific literature we know that muscle architecture, usually assessed by ultrasound, can influence maximal force production (Lieber and Fridén, 2000) and its transmission along the muscle-tendon unit (Narici and Maganaris, 2007), as well as affecting the relationship between force, muscle length, and contraction velocity (Gans, 1982; Timmins et al., 2016). Considering that skeletal muscle presents a remarkable degree of tissue plasticity in response to loading and unloading (Goldspink, 1985), focusing on muscle architectural adaptations occurring in remodeling scenarios may lead to insights into significant alterations in muscle function (Brughelli and Cronin, 2007; Lieber and Fridén, 2001). Recent investigations suggested that muscle architecture may play a role in muscular susceptibility to injuries (Bourne et al., 2017). In addition, other recent studies showed that muscle architecture changes to chronic loading could be specific to the modality of contraction used (i.e., eccentric vs. concentric) (Franchi et al., 2014; Reeves et al., 2009; Timmins et al., 2016).
However, ultrasonography technique presents some minor limitations, as images could be acquired with a limited field of view (i.e., small probes used in scans acquisition). This implies the use of equations or manual extrapolation of fascicle length for fascicles that may extend outside the field of view. Although the technique has been shown to be reliable by many investigations and it is scientifically accepted, we still lack universally accepted muscle models by which we could properly predict muscle function.
A good read I would suggest to check out is a comprehensive review by Prof Narici (1999), which will definitely help to better understand the significance of muscle architecture.
(A special thanks to Dr. Robert Csapo for the scientific discussion/contribution that helped to shape up these paragraphs).
Freelap USA: Remodeling of other tissues than muscle, such as tendon and ligament, is starting to become clearer with new research. Besides eccentric training, could you get into some suggestions of what coaches should know about these structures to help athletes come back after injury or recover smarter?
Martino Franchi: Tendon research during loading and unloading states is definitely increasing in the number of studies and publications. From the late ’90s, advancements were made through the use of ultrasound that allowed quantifying the tensile deformability of tendons (Maganaris et al., 2017). We now have data that shows tendon adaptations (mechanical properties and material remodeling) in response to different mechanical stimuli.
It seems that, in tendons presenting tendinopathy, both concentric and eccentric training have shown to have similar beneficial effects (Kjaer & Heinemeier, 2014). This suggests that, as long as a certain magnitude of load and strain is applied onto overused human tendons, and apparently at slower velocities, positive results are found whether someone adopts lengthening or shortening muscle actions as a main training strategy. Nonetheless, it is often assumed that these adaptations or mal-adaptations occur homogenously along the whole tendon length: A recent review (Maganaris et al., Frontiers in Physiology, 2017) instead nicely pointed out how specific regions of different tendons are subjected to more or less (or even none) mechanical stress during movement/training. The future tasks for researchers, coaches, and therapists would be to focus on individuating the real “internal stress-strain fields” in tendons, in order to strategically target the main degenerated regions with novel training approaches.
Freelap USA: Can you get into some practical advice for a very heavy topic such as molecular biology in sport? How much should a coach or therapist think about this? Is this the future or just a deeper understanding of the puzzle?
Martino Franchi: Molecular biology surely had a great impact on my research, but I personally think that it definitely influenced my view of what may or may not happen to skeletal muscle in different loading scenarios. In my experience as head of sport science/athletic trainer (2015-2016) of the Nottingham Wildcats Basketball Club (league winner of 2016 WBBL, Women’s British Basketball League), I had the pleasure to work alongside physiotherapist (and kinesiologist … and a good friend of mine), Aaron Wharton (give him a follow on twitter, @aaronmwharton). During many of our discussions, in which we brainstormed on how to best manage specific conditions of specific athletes (i.e., preventive and rehabilitation strategies, as well as loading interventions and periodization), molecular biology came up to surface quite a lot in my rationales. And what I loved is that Aaron was surprisingly interested and adjusted his physiotherapy approach to our thoughts/ideas.
So, in a sense, molecular biology is a deeper understanding of the puzzle, but I think it could be of help to coaches and therapists. But, buck it up: The molecular biology puzzle is immense, and not always that clear! Pick and choose what is scientifically sound and leave the noise out.
Freelap USA: Aging seems to be something that many coaches ignore at first because most athletes are typically not senior populations, but as athletes move past 30 things tend to change. Without suggesting more rest, what can coaches learn from aging studies to help the veteran athletes?
Martino Franchi: I think aging research is not entirely able to help the management of athletes past the age of 30. It’s definitely something that goes “each by each” for any athlete, and the variability within that age group is huge. Thus, aging science cannot do much for now, I am afraid.
Freelap USA: A lot of teams are doing concentric training to keep athletes from being sore during the competitive season, sometimes for months. In your research, you showed that muscle size may be the same over time, but the function may change. Can you advise coaches on how to manage the strain of eccentrics without resorting to pampering the athlete?
Martino Franchi: I had to read this question again and again, and frankly, I don’t see why eccentric training should be demonized like that. Not only when matched for relative maximum load (Reeves et al., 2009; Franchi et al., 2014) do concentric and eccentric training result in a similar increase in muscle size (even in short-term training periods—Franchi et al., 2015), but it looks like eccentric-induced muscle damage appears more in people who are unaccustomed to that type of training (and I think athletes should instead be quite customized to that!). It seems that the architectural adaptations to the two different training modes are contraction-specific, thus potentially resulting in different functional changes. Therefore, a coach may be prone to favor one type of training over the other, and rightly so, I would say.
Additionally, a recent study by Margaritelis and colleagues (2015) has shown that muscle damage and inflammatory response after eccentric training can be circumvented by an initial combination of concentric and eccentric stimuli, overcoming the repeated bout effect. Maybe it’s time to focus on what a coach wants most in terms of muscle structural and functional changes over time, thus choosing specific periodization strategies in training and rehabilitation programs (Harris-Love et al., Frontiers in Physiology, 2017).
Since you’re here…
…we have a small favor to ask. More people are reading SimpliFaster than ever, and each week we bring you compelling content from coaches, sport scientists, and physiotherapists who are devoted to building better athletes. Please take a moment to share the articles on social media, engage the authors with questions and comments below, and link to articles when appropriate if you have a blog or participate on forums of related topics. — SF